Inequalities in mental health, well-being and wellness in Canada
Trends in mental health inequalities in Canada. Highlights changes over time and drivers of mental health inequalities.
- Last updated: 2024-09-10
For a pdf copy of this report, please contact health.inequalities-inegalites.en.sante@phac-aspc.gc.ca
Download
the executive summary
(PDF format, 417 KB, 11 pages)
Published: 2024-09-10
On this page
1. Introduction
Mental health is an issue of increasing importance for people living in Canada, and it is becoming more widely discussed in civil society; it is also increasingly a public health priority Footnote 1 . The ability to respond to mental health issues, whether during health crises, climate change events, economic downturns, or other conditions, depends on a shared understanding of the contexts within which mental health inequalities can arise and how they have changed over time.
The focus of this report is to provide an overview of mental health inequalities by examining the structural and social determinants of health that contribute to mental health outcomes. The structural determinants of health encompass processes such as economic, and political mechanisms that give rise to disparities in between populations within society Footnote 2 . Social determinants of health are the nonmedical factors in our lives that affect our health—where we live; our income, education, job, and access to health care; and our social connections Footnote 2 . (Refer to Box 2.1 for more definitions of key terms).
Changes in mental health outcomes over time are assessed using measures of life satisfaction, perceived mental health, well-being, and mental illness. Also examined is whether mental health, as a whole and within specific populations, has improved or worsened. This report also aims to increase the understanding of how some root causes shape inequities in mental health outcomes.
The full set of results and data visualizations can be found on the accompanying online data tool tab at https://health-infobase.canada.ca/mental-health/inequalities/data-tool.html . This includes both positive mental health and mental illness outcomes.
1.1 Positionality Statement
This report was developed as part of the Pan-Canadian Health Inequalities Reporting Initiative (HIRI), a collaborative undertaking by the Public Health Agency of Canada (PHAC), the Pan-Canadian Public Health Network, Statistics Canada, the Canadian Institute for Health Information, and the First Nations Information Governance Centre (FNIGC) . The HIRI mandate is to strengthen measurement, monitoring, and reporting of health inequalities in Canada. The initiative supports surveillance and research, informs program and policy decision-making to reduce health inequities, and enables monitoring of progress in this area over time.
Initiated in response to the Rio Political Declaration on Social Determinants of Health Footnote 3 , this work is aligned with the Federal Anti-Racism Secretariat’s guiding values of justice, equity, human rights, diversity, inclusion, decolonization, integrity, anti-oppression, and reconciliation Footnote 4 and with the Federal 2SLGBTQI+ Action Plan to advance equality for Two-Spirit, lesbian, gay, bisexual, transgender, queer, intersex, and other sexual and gender-diverse (2SLGBTQI+) people in Canada Footnote 5 . This work also responds to the Truth and Reconciliation Commission’s nineteenth Call to Action to monitor the health inequities between Indigenous Peoples and non-Indigenous Canadians. Established in 2012, the HIRI has historically been informed by focusing on epidemiological data and methods, while incorporating social science and social epidemiological insights Footnote 6 , Indigenous worldviews Footnote 7 Footnote 8 Footnote 9 Footnote 10 Footnote 11 , and the social determinants of health framework developed by the World Health Organization ( WHO) Footnote 12 . The HIRI continues to use the same model of the social determinants of health—one that is also utilized internationally—to monitor inequalities in health outcomes and determinants among population subgroups of people living in Canada at the national, provincial, and territorial level and inform policy for health equity.
The HIRI is driven by an understanding that health inequalities cannot be addressed by the health sector alone. Employment, education, housing, and multiple other sectors need to jointly address social, economic, and political factors (for example, policies at various levels of government) that influence health, as well as the systems and structures that shape how these factors are distributed . Systemic forces refer to those which are manifested in each of society’s major parts, including the economy, politics and religion while structural forces refer to specific structures, such as laws, policies, institutional practices Footnote 156 . Both systemic and structural forces, such as racism, colonialism, xenophobia, heterosexism, ableism, and discrimination, generate and reinforce societal hierarchies, distributions of power and resources, and opportunities that inform and influence the social and material conditions into which individuals are born, grow, live, work, play, and age Footnote 13 . Tackling health inequalities requires a multilevel approach that includes policy interventions at the highest or macro level, through upstream action that redistributes opportunities for health in ways that are just for all, and at the meso level, through policy interventions in schools, communities, health services, and other settings.
After continued engagement with partners across federal government departments, national Indigenous organizations, and experts outside of PHAC, the HIRI has sought to enhance integration of Indigenous worldviews as well as feminist, intersectional, and decolonizing approaches in the planning and development of its reporting practices Footnote 14 . The HIRI continues to strive to integrate interdisciplinary theories and methodologies when monitoring and measuring health inequalities in Canada. This report is enriched by qualitative evidence gleaned from studies that used various methodologies such as participant observation, structured interviews, and other forms of fieldwork.
1.2 Aims and Objectives
1.2.1 Why focus on mental health?
Problems related to poor mental health affect individuals and the people around them and has far-reaching economic and societal implications. As a leading cause of disability in Canada Footnote 15 , poor mental health leads to greater absenteeism in the workplace and reduced productivity Footnote 15 . The financial costs of poor mental health, including mental illnesses, are substantial, at approximately $51 billion each year in health care expenditures and lost productivity Footnote 15 . The burden of mental health, in terms of economic and societal costs, increases when levels of high self-rated mental health are lower in the population.
Families frequently experience increased stress and disruption in daily life as well as financial difficulties as a result of supporting family members with mental health–related problems. Mental illness can contribute to social isolation and withdrawal from social activities, which can lead to decreased community engagement and strained relationships Footnote 16 , and, in turn, contribute to a cycle of poor mental health. Further, the stigma associated with mental illness and poor mental health in general can lead to discrimination, social exclusion, and reduced quality of life.
Taken together, the societal and economic toll of mental health is substantial. A comprehensive understanding of inequalities in mental health outcomes and their determinants is essential to developing strategies and interventions to improve the mental health of people in Canada.
1.2.2 Why focus on mental health inequalities?
Health equity is embedded in the World Health Organization (WHO) Constitution and the Universal Declaration of Human Rights Footnote 17 . The former proclaims that “the highest standards of health should be within reach of all, without distinction of race, religion, political belief, economic or social condition” while the latter states that “everyone has the right to a standard of living adequate for the health and well-being of himself and of his family, including food, clothing, housing and medical care and necessary social services, and the right to security in the event of unemployment, sickness, disability, widowhood, old age or other lack of livelihood in circumstances beyond his control”. Health equity is concerned with creating equal opportunities for health for each member of a society. Advancing health equity means working towards eliminating unfair and avoidable differences between socially advantaged and disadvantaged groups that have poorer health status and shorter lives, a role for many within and outside the health sector Footnote 18 . One way to do so is to focus on systems and structures of power affecting different populations through the distribution of material and social resources within societies, known as social determinants of health. The social determinants of health refer to the conditions which we are born into, where we grow up, where we live, how and in what ways we work, and even how we spend our free time. They encompass the broader societal, economic, and environmental influences that significantly impact individual and community health outcomes, extending far beyond healthcare access and directly shape our overall health, including mental health.
According to the WHO Footnote 2 , the social determinants of health (such as income, employment, and housing) and the broader factors that shape living and working conditions account for between 30% and 55% of health outcomes, a much greater effect than lifestyle choices and activities (e.g., exercise). Compared to the health care system, our education, justice, and social welfare–related socioeconomic systems and political contexts have been found to contribute significantly to health outcomes Footnote 2 Footnote 19 Footnote 20 :
As we conceptualize these deeper layers, the core social determinants of mental health can be understood as stemming directly from unequal distribution of opportunity. Although it may affect individual patients and may be considered in formulations and intervention planning based on the biopsychosocial model, this unequal distribution of opportunity is primarily a concern about society. As such, it is a social justice issue, rather than a clinical issue. Social justice means fair distribution of advantages and equal sharing of burdens while focusing on those most disadvantaged. Footnote 21
Monitoring health inequalities over time is important in order to support public health actors, such as health professionals, community leaders, and others with an interest in the drivers of mental health inequalities; and public sector actors, for example , politicians, public servants, community organizations, and nongovernmental organizations that assess whether policies and programs contribute to or mitigate inequalities. This requires an improved understanding, description, and response to health inequalities to address the fundamental determinants of health and promote social justice and health equity Footnote 14 .
Various models have been developed to map and understand how determinants of health influence health outcomes. Informed by the WHO conceptual framework Footnote 12 , PHAC defines social determinants of health as the “social and economic factors … that relate to an individual’s place in society” Footnote 22 . The conceptual framework for action on the social determinants of health developed by WHO (shown in Figure 1) has 2 levels of determinants: structural and intermediary .
The first level or structural-level determinants shape conditions for health through socioeconomic and political contexts. Social, economic, and other institutional policies, systems, and values shape health and well-being through the ways that power, resources, and opportunities are distributed within and between populations Footnote 13 Footnote 23 . Societal values—including prejudice and stigma towards populations or people with certain health conditions Footnote 24 —influence prevention opportunities and treatment options. In addition, broader economic and ideological systems, such as capitalism Footnote 25 , systemic racism, colonialism, sexism, heterosexism, and ableism Footnote 26 underlie policy approaches that influence social determinants of health, through decisions made regarding education, housing, the labour market, and societal protections. The structural determinants of health shape the socioeconomic position of individuals and of populations within society. This position is further affected by education, occupation, ethnicity, race, sex, gender expression, and sexual orientation, among others Footnote 13 Footnote 23 .
These structural determinants influence the second level or intermediary-level determinants of health. Intermediary determinants include factors related to the health system (e.g., health service availability, accessibility, uptake) and access to health-promoting social and material resources and opportunities, including the built environment, food environments, workplaces, and homes Footnote 13 Footnote 23 Footnote 26 .
In Canada, research has documented associations between various mental health outcomes and markers of social position such as age, sex, gender expression, sexual orientation, ethnicity, race, income, education, and employment status Footnote 13 Footnote 26 Footnote 27 Footnote 28 as well as intermediary factors such as food security, access to mental health care, quality of social ties, discrimination, stigma, and violence Footnote 24 Footnote 27 Footnote 29 Footnote 30 .
Figure 1. Conceptual Framework for Action on the Social Determinants of Health (Solar & Irwin, 2010)
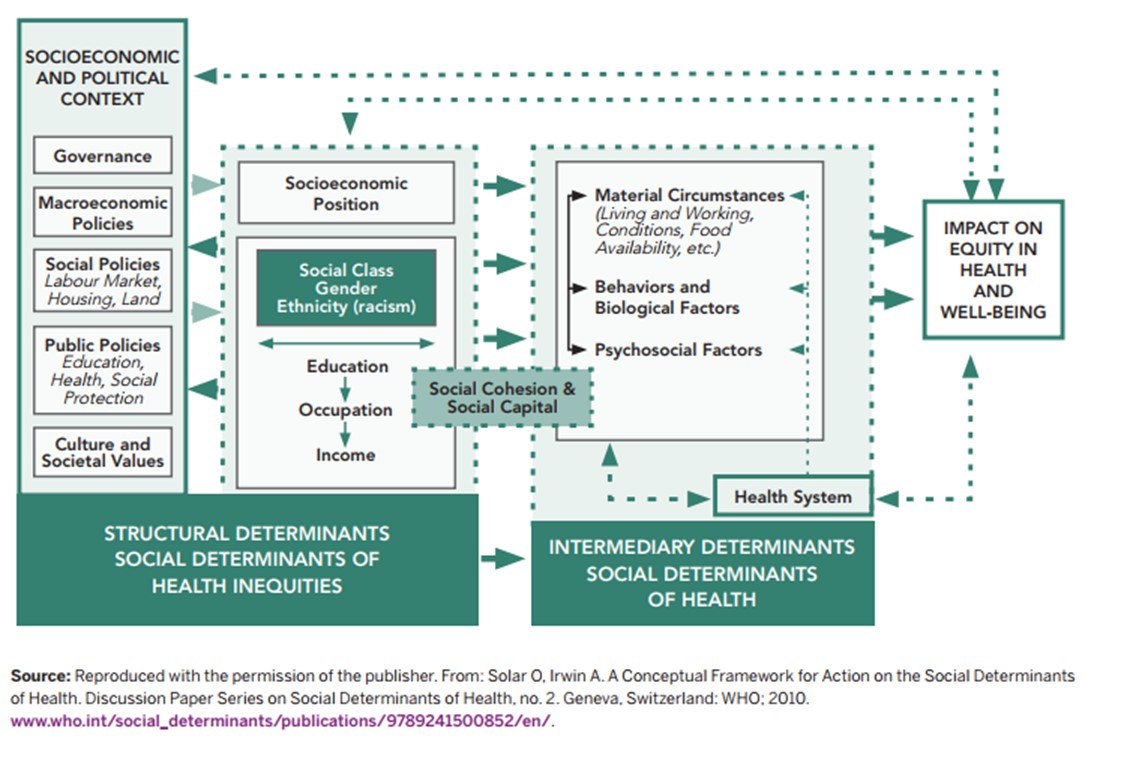
Figure 1: Text description
Using arrows, the framework indicates the interconnections and cyclical nature of measures concerning the social determinants of health. The framework consists of two main parts (parts A and B).
Part A, entitled “Structural Determinants, Social Determinants of Health Inequities”, comprises two main sub-sections. The first deals with the socioeconomic and political context, and includes governance, macroeconomic policies, social policies (labor market, housing and land), public policies (education, health, social protection) and societal culture and values. The second sub-section concerns socio-economic status, including social class, gender, ethnic origin (racism), education, employment and income. These two subsections are linked by bidirectional arrows.
Part B, entitled “Intermediate Determinants, Social Determinants of Health”, comprises three elements: material conditions, including living and working conditions, availability of food, etc.; behaviours and biological factors; psychosocial factors. The “health system” is also considered an element of Part B, but it appears in a separate box, linked by a bidirectional arrow to the main components of Part B.
One-way arrows link Part A to Part B, and a “Social cohesion and social capital” box also links these two sections.
Unidirectional arrows link Part B, in particular the “Health system” box, to a box on the far right of the diagram entitled “Impact on health equity and well-being”. Finally, two unidirectional arrows lead from the “Impact on health equity and well-being” box to the two main subsections of the “Structural Determinants, Social Determinants of Health Inequities” section (part A).
“Both public policies and social norms are structured such that they favour some individuals and groups over others, which sets the stage for the unequal distribution of opportunity, and thus the social determinants of mental health. Although clinical interventions clearly have a role in reducing risk for mental disorders, the greatest population-based impact for preventing many chronic physical health conditions and a number of mental disorders and substance use disorders would be achieved by optimizing public policies to make them more health promoting and by shifting social norms so that together we prioritize the health of all members of society.” Footnote 21
The pathways through which social determinants of health impact mental health and well-being can include events and conditions that are physiological and psychological stressors. Large-scale events, such as natural disasters, and individual-level circumstances, such as violence or material deprivation, can result in biophysical responses that negatively affect immune, metabolic, and endocrine systems Footnote 28 in addition to emotional and psychological well-being Footnote 28 . Individuals may turn to coping behaviours to mitigate these effects; these behaviours can be health promoting (e.g., meditation, exercise) or harmful (e.g., problematic substance use). However, the behaviours are always adopted in the context of the influence of social norms, values, life-stage factors, identity factors (e.g., gender, religious affiliation), availability of and access to supports, and so on, and they play a role in the intensity and duration of the impact of social determinants on one’s mental health.
Guided by the Commission on Social Determinants of Health (CSDH), established by WHO, the HIRI primarily utilizes cross-sectional quantitative data to monitor health inequalities. We expand on previous reporting by examining both quantitative and qualitative evidence. Through a process of thematic analysis and synthesis of the findings of Canadian qualitative studies, and quantitative analyses of nationally representative survey data describing mental health inequality trends between 2007 and 2022, our aim was to develop a portrait of the key social and structural determinants of mental health and well-being in Canada.
This report pays special attention to upstream determinants including the socioeconomic, political, cultural, historical, and environmental factors that affect the mental health and well-being of people living in Canada. Although these upstream factors have often been considered removed from health outcomes, in fact they have profound impacts on health disparities and outcomes. Addressing upstream factors requires looking at systemic or societal issues, such as poverty, discrimination, access to education, and an equitable distribution of other resources. In integrating interdisciplinary perspectives and approaches, this report aims to broaden understanding of mental health and well-being.
In addition, this report has an accompanying online data tool that provides a comprehensive repository of mental health inequality trends to expand and complement the analyses presented in this report. This tool can be found at https://health-infobase.canada.ca/mental-health/inequalities/data-tool.html .
2. How is Mental Health Conceptualized in Canada ?
Mental health has been defined in many ways, with each definition influenced by social and cultural contexts Footnote 30 . Globally, there is no official consensus on a singular definition of mental health, and core concepts vary depending on different theories, models, and paradigms Footnote 31 .
In this section we summarize various common mental health constructs taken into account in this report.
2.1 Why Reflect on Definitions of Mental Health?
Several interdisciplinary health and social theories inform the HIRI and this report. One of these is intersectionality theory, a central principle of which is the importance of recognizing different forms or types of knowledge and ways of knowing Footnote 32 Footnote 33 . In the domain of public health, this can be applied by reflecting critically on the forms of knowledge that are considered valid and valuable in public health decision-making Footnote 14 .
A primary aim of this report is to explore how mental health is conceptualized in Canada, across epistemological perspectives and traditions. Broadly, this report understands mental health as an umbrella term that includes both positive and negative states of mental health.
Systematic exclusion of certain types and sources of evidence or voices can intentionally or unintentionally perpetuate the marginalization of certain communities and contribute to ongoing health and social inequalities. For example, if the people responsible for shaping policies and programs and the intended beneficiaries of these programs and policies are not involved in evidence synthesis and decision-making, the programs and policies may be designed in ways that do not meet the distinct needs of the communities they are meant to serve Footnote 32 . To counter this tendency, best practices in public health research and surveillance consider multiple ways of knowing and types of knowledge when defining key terms, issues, and concepts Footnote 14 . In this report, exploring how various sources, communities, or systems of knowledge production define or understand mental health can provide depth and nuance to mental health promotion initiatives.
Box 2.1. Key Terms and Their Definitions
|
Terms |
Definitions |
|
Health Inequalities |
Refer to differences in health status or in the distribution of health determinants between different population groups. These differences can be due to biological factors, individual choices, or chance. Nevertheless, public health evidence suggests that many differences can be attributed to the unequal distribution of the social and economic factors that influence health (e.g., income, education, employment, social supports) and exposure to societal conditions and environments largely beyond the control of the individuals concerned. |
|
Health Inequity |
Health inequity refers to differences in health associated with structural and social disadvantage that are systemic, modifiable, avoidable and unfair. Health inequities are rooted in social, economic and environmental conditions and power imbalances, putting groups who already experience disadvantage at further risk of poor health outcomes Footnote 34 . |
|
Health Equity |
Health equity means that all people (individuals, groups and communities) have fair access to, and can act on, opportunities to reach their full health potential and are not disadvantaged by social, economic and environmental conditions, including socially constructed factors such as race, gender, sexuality, religion and social status. Achieving health equity requires acknowledging that some people have unequal starting places, and different strategies and resources are needed to correct the imbalance and make health possible. Health equity is achieved when disparities in health status between groups due to social and structural factors are reduced or eliminated Footnote 34 . |
|
Social Determinants of Health |
The social determinants of health are the interrelated social, political and economic circumstances in which people are born, grow up, live, work and age. The social determinants of health (see below) do not operate as a list or in isolation. It is how these determinants intersect that causes conditions of daily living to shift and change over time and across the life span, impacting the health of individuals, groups and communities in different ways Footnote 34 . |
|
Structural Determinants of Health |
Structural determinants of health are processes that create inequities in money, power and resources. They include political, cultural, economic and social structures; natural environment, land and climate change; and history and legacy, ongoing colonialism and systemic racism. Structural determinants, also known as structural drivers, shape the conditions of daily life (social determinants of health) including education, work, aging, income, social protections, housing, environment and health systems Footnote 34 . |
|
Downstream (Micro) approaches |
Downstream interventions and strategies seek to address immediate needs and mitigate the negative impacts of disadvantage on health at an individual or community level through the availability of health and social services. These changes generally occur at the service or access-to-service level. Downstream strategies are about changing the effects of the causes Footnote 34 . |
|
Midstream (Meso) Approaches |
Midstream interventions and strategies reduce exposure to risk by improving material conditions or by promoting healthy behaviours. These changes generally occur where individuals who live with inequities are directed or referred to resources that support health at the regional, local, community or organizational level. Midstream approaches are about changing the root causes of health inequities Footnote 34 . |
|
Upstream (Macro) Approaches |
Upstream interventions and strategies dismantle and change the fundamental social and economic systems (structural determinants of health) that distribute the root causes of health inequities including wealth, power and opportunities. These changes generally happen at the provincial, territorial, national and international levels. They are about changing the cause of the causes of health and health inequities Footnote 34 . |
|
Intersectionality |
Intersectionality considers how systems of oppression (e.g., racism, classism, sexism, homophobia) interact to influence relative advantage and disadvantage at individual and structural levels. An intersectional orientation recognizes that the experience of multiple forms of discrimination and disadvantage has a cumulative negative effect that is greater than the sum of the parts. The intersectional nature of oppression and privilege means that people may have privilege in one or more forms even if they experience oppression in other domains Footnote 34 . |
|
Mental Health |
Refers to an umbrella term that encompasses an individual’s state of well-being (emotional, psychological, social), measured by levels of positive mental health (i.e., self-rated mental health, happiness, life satisfaction, psychological and social well-being) and/or experiences of mental health problems or mental illness (i.e., anxiety disorders, mood disorders, substance use disorders or others). |
|
Mental Illness (also known as Mental Disorders) |
Refers to a wide range of conditions that affect a person's thinking, emotions, behaviour, or mood. These conditions can vary in severity, duration, and impact on daily life. Mental illnesses can encompass various disorders such as depressive disorders, anxiety disorders, schizophrenia, bipolar disorder, posttraumatic stress disorder (PTSD), obsessive-compulsive disorder (OCD), and many others. |
|
Poor Mental Health or Problems related to Mental Health |
Refers to the presence of a negative state of mental health and can be used as general terms for mental distress, and/or mental disorders, and/or mental illness, and/or substance use disorders, and/or suicidality. Importantly, an individual can have poor mental health or problems related to mental health without necessarily having a mental illness. |
|
Positive Mental Health |
Refers to the presence of a state of positive mental health. The PHAC definition of positive mental health is “The capacity of each and all of us to feel, think, act in ways that enhance our ability to enjoy life and deal with the challenges we face. It is a positive sense of emotional and spiritual well-being that respects the importance of culture, equity, social justice, interconnections and personal dignity” Footnote 35 . |
|
Two-Spirit
|
The term “two-spirit” is used by some Indigenous People to refer to persons who identify as having both a masculine and a feminine spirit. The term describes a person’s sexual, gender and/or spiritual identity. Persons who identify as two-spirit may be attracted to persons of the same sex and/or may identify as gender diverse, and include people who in Western culture may be described as gay, lesbian, bisexual, and transgender, among others. The term “two-spirit” was introduced by Elder Myra Laramee during the Third Annual Inter-tribal Native American, First Nations, Gay and Lesbian American Conference, held in Winnipeg in 1990. |
|
Social Gradient in Health |
Refers to the consistent, incremental differences in health outcomes or status that correspond to variations in socioeconomic status or other social determinants. These gradients illustrate how health tends to improve as socioeconomic status rises, showcasing a stepwise pattern where individuals with higher social or economic positions generally experience better health compared to those in lower positions. |
|
Cross-cultural Validity |
Refers to the extent to which a concept, assessment, or measurement tool is meaningful, relevant, and accurately measures what it intends to across different cultures or cultural groups. It ensures that the tool or assessment is fair, reliable, and doesn't disproportionately favour or disadvantage any particular cultural group when used in diverse cultural contexts. |
|
Health Promotion |
Health promotion is the process of enabling people to increase control over, and to improve, their health. It moves beyond a focus on individual behaviour towards a wide range of social and environmental interventions. As a core function of public health, health promotion supports governments, communities and individuals to cope with and address health challenges. This is accomplished by building healthy public policies, creating supportive environments, and strengthening community action and personal skills Footnote 36 . |
2.1 Biomedical Definitions of Mental Health
The biomedical model of mental disorders presumes that there are biological causes for abnormalities in the brain that result in mental illness. Contextual factors such as social interactions, resources, systems, and determinants are not considered Footnote 37 Footnote 38 , and biomedical conceptualizations of mental illness and health typically centre on mental distress, illnesses, and disorders or conditions and tend to focus on their etiologies, diagnoses, and remediation with psychotherapeutic treatments.
From a clinical diagnostic and treatment perspective, mental illnesses (or disorders) refer to emotions, mood, difficulties in thinking, and/or behaviours that impede a person’s day-to-day functioning Footnote 39 . Mental illnesses are defined by the Diagnostic and Statistical Manual of Mental Disorders (DSM) and the International Classification of Diseases (ICD) Footnote 40 Footnote 41 . The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders describes more than 150 clinical mental diagnoses, such as major depressive disorder and generalized anxiety disorder Footnote 42 and includes diagnostic criteria for conditions such as schizophrenia, bipolar and related disorders, trauma- and stressor-related disorders such as posttraumatic stress disorder (PTSD), substance-related disorders such as alcohol use disorder, and eating disorders.
Biomedical definitions of mental health and illness tend to dominate among epidemiologists, policy analysts, researchers, and health management officials Footnote 43 , who focus on individual-level attributes and behaviours and prioritize individual-level measures Footnote 38 .
2.2 Mental Health Models
Some scholars have proposed that mental health exists on a continuum from poor to good, on which a person can move between effective functioning to severe and persistent functional impairment Footnote 44 . Shifts along this mental health continuum can occur in response to biological, psychological, social, and economic factors, as well as specific life stressors. Mental health is thought of as the absence of mental illness Footnote 45 Footnote 46 . This polar relationship between mental health and mental illness has been the basis of psychological and psychiatric understanding and assumptions Footnote 47 .
In contrast, the dual continua model views mental health and mental illness as interrelated but distinct phenomena, with positive and negative effects, that operate independently of each other Footnote 47 . A person can have good mental health even if they have a mental illness (or disorder). They can experience elements of both mental illness and mental health, physically or emotionally, at different times or concurrently.
In 2021, 1 in 3 people aged 15 years and older had experienced a mental illness or substance use disorder during their lifetime Footnote 48 . Further, 9.6% of the population aged 12 years and older reported having a diagnosed mood disorder Footnote 49 . However, individuals with a diagnosed mood and/or anxiety disorder or substance use disorder can still self-rate their mental health or life satisfaction as high Footnote 50 .
2.3 Positive Mental Health
PHAC defines positive mental health as “the capacity of each and all of us to feel, think, act in ways that enhance our ability to enjoy life and deal with the challenges we face. It is a positive sense of emotional and spiritual well-being that respects the importance of culture, equity, social justice, interconnections and personal dignity” Footnote 51 . As such, positive mental health is considered necessary to flourish Footnote 44 . It is also an integral component of the WHO definition of health as a “state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity” Footnote 17 . Positive mental health also has proven effects on biological functioning, cardiovascular risk, and improved immunity Footnote 43 .
The components of positive mental health are multifaceted and include functioning (e.g., motivations) and positive affect (e.g., happiness), strengths, self-actualization, personal capacities, and existentialist approaches with eudemonic (e.g., positive experiences) and hedonic focuses (e.g., meaning in life) Footnote 43 .
In 2016, in consultation with the Mental Health Commission of Canada (MHCC), PHAC developed a conceptual framework to strengthen surveillance of positive mental health and its determinants Footnote 52 . The Positive Mental Health Surveillance Indicator Framework (PMHSIF) includes 5 outcome indicators and 25 determinant indicators spanning the 4 contextual domains of individual, family, community, and society. Positive mental health outcomes include self-rated mental health, life satisfaction, happiness, psychological well-being, and social well-being.
Interventions that support the mental health of populations should focus on promoting positive mental health by addressing the social and structural determinants to complement illness prevention, treatment, and support. The Canadian Mental Health Association (CMHA) develops strategies to ensure equitable mental health care across the life course and within communities, focusing on mental health promotion, prevention, and early intervention Footnote 327 .
In 2021, around 60% of adults and youth aged 12 to 17 years reported very good or excellent mental health and 73% reported being usually “happy and interested in life” Footnote 35 . On average, adults and youth reported being relatively satisfied with their lives, with about one-third of adults and about one-half of youth reporting being “very satisfied” Footnote 35 .
Risk and protective factors, from the individual to the societal level, contribute to positive mental health. Individual determinants, for example, physical activit y, substance use (and, for youth, substance use by family members), resilience, and coping, can influence an individual’s positive mental health. Similarly, family determinants such as family relationships, parenting style (for youth), household composition, and household income can promote positive mental health. Community determinants include social support and networks, school and work environment, and neighbourhood environment. Mental health determinants a t the societal level include social justice, and discrimination and stigma. As such, positive mental health measures are most often subjective; although theoretical in nature, the measures have been empirically validated Footnote 43 .
2.4 Expanding the Definition of Mental Health
How mental health is understood and defined is both historically and culturally contingent. Considering Canada’s Indigenous population and its distinct ways of knowing and being , its historical and current immigration policies, and its culturally and socioeconomically diverse populations, conceptualizations, definitions, and experiences of mental health vary widely. However, existing policies, programs, and initiatives intended to address mental health rarely consider this diversity. Overall, existing initiatives and treatments mostly reflect dominant biomedical science and evidence-based medical practice. These mental health narratives are primarily derived from clinical and psychological research focused on middle-class, educated, younger Western populations Footnote 53 . Scholars have pointed out how the nature and production of evidence-based medicine is influenced by and reproduces systems of power and privilege, such as patriarchy and sexism, racism, colonialism, heterosexism, ableism, and classism and does not reflect the cultural diversity of countries like Canada Footnote 53 .
To address this limitation, it is necessary to acknowledge Canada’s heterogeneous population and consider systems of power, the broader social context, and intersecting determinants of mental health shaped by people’s respective needs and experiences to both understand how social and structural factors shape mental health and how to achieve equity Footnote 54 .
Indigenous perspectives on mental wellness acknowledge these and other factors to provide a more inclusive and holistic conceptual framework. “Wellness” in many Indigenous communities and cultures across Canada is understood to encompass mental, physical, spiritual, and emotional balance. Thus, wellness focuses on strengths rather than deficits, and highlights the role of social and cultural environments. This contrasts with mainstream western understandings of health, which as discussed in previous sections, largely focus on biological causes for abnormalities that cause illness. For this reason, in the context of discussing Indigenous perspectives, the discussion is framed around “mental wellness” rather than “mental health.”
Indigenous Peoples possess distinct and diverse worldviews that often embrace holism, relationality, circularity, and interconnection Footnote 8 Footnote 55 Footnote 56 Footnote 57 . Although they represent distinct cultural groups, a common perspective shared by many First Nations, Inuit, and Métis Peoples is that health and wellness involve a balance of physical, mental, emotional, and spiritual aspects of life Footnote 58 Footnote 59 . In the following sections, we have taken a distinctions-based approach to exploring different understandings of mental wellness. Informed by a number of discussions with national Indigenous organizations, the sections reflect complementary but distinct ways of conceptualizing mental wellness.
2.4.1 First Nations
The First Nations Mental Wellness Continuum Framework Footnote 11 provides a comprehensive definition of mental wellness as a balance of the “mental, physical, spiritual, and emotional” Footnote 11 . The 4 dimensions are interconnecting and necessary for mental wellness at the individual, family, and community level. This balance is enhanced when individuals have purpose, hope, a sense of belonging, and a sense of meaning, all of which are key wellness outcomes.
From this perspective, mental wellness is supported by a number of layers and interconnected elements, with culture providing the foundation. Although different First Nations express and experience culture in different ways, there are some shared core beliefs and concepts: the Spirit (an inclusive concept of body–mind–heart–spirit ); the Circle (the patterns of life); Harmony and Balance; All My Relations (interconnectedness with people and nature); Kindness/Caring/Respect; Earth Connection; Path of Life Continuum; and Language. Culture, therefore, “is the expression, the life-ways, and the spiritual, psychological, social, material practice of this Indigenous worldview” Footnote 60 . First Nations’ culture and languages reflect a unique worldview that informs individual identities and their relationship with all aspects of creation. In this manner, culture guides First Nations’ unique ways of seeing, relating, being, and thinking. The knowledge contained within culture provides the foundation for individual and collective wellness and provides guidance across the life course.
2.4.2 Inuit
The Inuit-Specific Mental Wellness Framework defines mental wellness as “self-esteem and personal dignity flowing from the presence of a harmonious physical, emotional, mental, and spiritual wellness and cultural identity” Footnote 7 . From this perspective, mental wellness is not a singular concept; it encompasses mental health and mental illness, and aims to prevent violence, suicide, and harmful substance use Footnote 7 . The National Inuit Suicide Prevention Strategy expands upon this understanding of mental wellness by also recognizing the role played by resilience as “a resource that grows through an accumulation of protective factors, sometimes called health assets, which contribute to positive mental wellness, increased ability to deal with stress or adversity, and resilience-building behaviours” Footnote 61 .
Building protective factors that contribute to developing abilities, skills, and social supports that offer people the capacity to cope with stress and spring back from crises and trauma is an important component of the wellness concept. The National Inuit Suicide Prevention Strategy outlines some of these protective factors: coping with acute stress; family strength and support; optimal nurturing development; cultural continuity; social equity, and access to Inuit-specific mental health and wellness services and supports. Social equity is achieved by addressing the social determinants of Inuit health, namely quality early childhood development, culture and language, livelihoods, income distribution, housing, safety and security, education, food security, availability of health services, mental wellness, and the environment Footnote 61 .
For Inuit, the land carries great importance. Close connection with the land, nature, and harvesting activities is thought to promote overall health as well as mental wellness Footnote 62 . Eating country foods and spending time on the land helps establish and maintain a strong cultural identity, which is also considered a key protective factor for mental wellness Footnote 61 . Cultural continuity, which is another key protective factor in the Inuit wellness concept, can be supported via sustainable approaches to connecting Inuit with the land, culture, and language.
2.4.3 Métis
While the Métis National Council does not currently have a framework focused specifically on mental wellness, Métis communities, institutions, and Knowledge Holders continue to share their mental wellness knowledge throughout the Métis Homeland, including through reports and academic writing. For Métis people, health and wellness encompass not only physical health, but also a “state of balance and interconnected relationships between physical, mental, emotional, social, financial/economic, spiritual, environmental, and cultural well-being” Footnote 63 . Understandings of health and wellness are closely tied to connection with family and the wellness of others within kinship networks Footnote 56 . This worldview encompasses a connection to all things, including the land itself, all life on earth, other people, and a sense of identity and belonging Footnote 64 Footnote 65 . Traditional Knowledge, language, and cultural identity are foundational to health and mental wellness Footnote 9 . Engagement in cultural practices is seen as an important tool for promoting mental wellness, fostering cultural pride, self-esteem, and a sense of belonging Footnote 66 .
2.5 Differences and Similarities Across Definitions
In summary, there is no single definition of mental health. Definitions often differ based on whether mental health is being conceptualized as a state (e.g., mental illness), a dimension of health (e.g., mental health vs. physical health), by domain or discipline (e.g., psychiatry or public health), or even a social movement (e.g., mental hygiene). Conceptualizations have since been broadened to consider mental health as a domain of overall health and well-being, catalyzing more holistic, upstream, strengths-focused, and positive approaches. The WHO statement that “there is no health without mental health” Footnote 1 reflects this milestone.
3. Methodologies
This report used a range of methods to develop understanding of the structural determinants of mental health and drivers of mental health inequalities to address the overarching objectives of monitoring health inequalities . These are described in detail in the Technical Notes ( https://health-infobase.canada.ca/mental-health/inequalities/technical-notes.html ). In this section we describe the guiding framework of this project, intersectionality theory, which informed the decision to incorporate both qualitative and quantitative evidence in this report, and the literature reviews of both qualitative and quantitative evidence on the social determinants of mental health in Canada and trend analysis that summarizes patterns in national health survey data across time.
3.1 Intersectionality Theory as the Guiding Framework
Intersectionality theory and practice provided the guiding framework for this project. Emerging from early race, class, and gender analytical frameworks, intersectional approaches continued to develop in the crucible of the civil rights movement and Black feminist scholarship Footnote 67 Footnote 68 Footnote 69 Footnote 70 . Responding to the interlocking systems of anti-Black racism, sexism, heterosexism, and class oppression, intersectionality has been defined as a theory, a broad-based knowledge project, a research paradigm, an analytic framework, and a critical praxis. Intersectionality focuses on social inequality (e.g., oppression, discrimination, marginalization, and stigma) by paying attention to intersecting systems of power and privilege (e.g., racism, sexism, heterosexism, colonialism) Footnote 67 Footnote 71 . It references the critical insight that social positions such as race, ethnicity, class, sex, gender, sexual orientation, ethnicity, nationhood, ability, and age cannot be conceptualized as—nor operate as—unitary, mutually exclusive entities, but as relational and reciprocal social formations that cannot be separated Footnote 72 . Intersectionality emphasizes a need to consider and examine the ways in which interconnected systems and structures of power and oppression operate across time, place, and societal levels, contributing to unequal material realities and complex social inequalities Footnote 14 Footnote 32 Footnote 73 .
For this report, we bridged conceptual and methodological tools to better understand mental health inequalities in Canada, with the goal of examining these inequalities from new angles, specifically paying attention to systems of power. In particular, we focused on the core tenets of intersectionality theory, including: 1) an emphasis on the importance of equity (i.e., fairness) and social justice (i.e., the need for transformational change or action to challenge and address social inequalities) Footnote 74 ; 2) an understanding that social identities and hierarchies are constructed by systems of power; 3) critical reflection on what types of knowledge or evidence are considered valid and who participates in producing the knowledge used in decision-making; and 4) recognition that knowledge production, sociopolitical contexts, health determinants, and outcomes can vary over time Footnote 32 .
Communities living in vulnerable circumstances or experiencing disadvantages are often excluded from processes of knowledge production. Consequently, intersectional knowledge projects try to include diverse and appropriately represented voices, worldviews, and forms of knowledge (e.g., experiential, traditional, scientific) in decision-making processes in order to disrupt the reproduction of socially dominant modes of knowledge production hierarchies. Intersectionality explores various theories of knowledge to consider how concepts are understood and defined; it discusses how determinants of health (along axes such as race/ethnicity, sex/gender, class, sexual orientation) intersect or overlap with one another to shape health outcomes and the inequalities therein, over time and across contexts; it engages with concepts of power; and, overall, it provides evidence to help address structural determinants of health and reduce health inequalities.
Accordingly, this report incorporates both qualitative and quantitative evidence, exploring the tenets of intersectionality of seeking out, honouring, and bringing into conversation different forms of knowledge, engaging with a myriad of experts and partners throughout the research design process, and developing the narrative in conjunction with a steering committee comprising community-based, academic, and public policy actors (membership is shown in the acknowledgements section), who provided direction and feedback throughout the process.
Still, there is room for improvement. For example, directly engaging with and co-producing research with Traditional Knowledge Keepers, communities, and/or repositories would go beyond the conventional sources of peer-reviewed publications and academic voices that make up the majority of the evidence presented in this report.
3.2 The Role of Qualitative Research in Understanding Mental Health Inequities
Qualitative research methodologies contribute to knowledge and discourses that are not standardized and singular, providing rich descriptions of multidimensional experiences Footnote 75 Footnote 76 . In this report, qualitative studies have been synthesized to provide a larger context for differences in population based surveys in order to gain greater insight into the nature of mental health inequalities. Our use of qualitative evidence was purposeful and critical to examine the types of ideas underpinning how mental health was described and understood in different settings with multiple populations. Part of this exercise was to examine the theoretical perspectives that were the basis of the studies to see how authors framed the multiple dimensions that contribute to mental health. By applying an analysis that was guided by an intersectional approach, we paid special attention to the nuance and complexity of both social locations, contexts and of power relations that impact mental health (for example, negative experiences of certain populations in accessing care). Further, the adoption of a narrative synthesis of qualitative themes to guide the structure of the report adheres to the interpretive nature of qualitative methodologies, and thus reorients the report to enable examining structural and system-level contributions to mental health inequalities in Canada.
3.2.1 Qualitative Research Methods
For the qualitative component of the report, we conducted a rapid review Footnote 77 of qualitative studies of the social determinants of mental health and mental health inequalities from a Canadian public health perspective. The studies were published in a 10-year period (2012–2022). Searches spanned a spectrum of mental health terms (from positive to negative). However, it is important to recognize that the focus of health inequalities research has historically been deficit-based and qualitative results may reflect this perspective. The rapid review included peer-reviewed research that employed a variety of qualitative methodologies and focused on participants’ lived experiences of mental health to understand the complex contexts of mental health inequalities. A Health Canada librarian helped devise the search strategy and compile materials. Strict inclusion criteria were utilized, concordant with the research team’s capacity, to limit the review.
We adopted a staged and iterative literature search process to familiarize ourselves with the main topics of study, subpopulations, and the theoretical perspectives in research on inequalities in mental health. Since the focus was on peer-reviewed research published in academic journals, a publication bias might exist within the evidence synthesis. However, this initial review was supplemented with additional literature searches and other forms of knowledge were included, where necessary. Sources consulted for the sections focused on First Nations, Inuit, and Métis were identified through discussions with our Indigenous partners or using targeted searches for the topic of interest.
We followed a process of narrative synthesis to derive key themes in the body of evidence reviewed Footnote 76 . The goal of this process was to generate new insights by amalgamating study findings. Using an inductive approach, we extracted and synthesized the findings from 67 Canadian studies (out of a total of 588 initially identified). Key themes derived from the qualitative synthesis were: socioeconomic conditions; racism, xenophobia, homophobia, and other types of discrimination; social and cultural connection, support networks, and community belonging; and access, quality, and use of health care services. We conducted a supplementary search as a validation exercise to ensure that these 4 themes were consistent with systematic reviews of social determinants of mental health beyond the 10-year period initially searched. We found that the 4 identified qualitative themes were well represented and validated by the supplemental search Footnote 78 Footnote 79 Footnote 80 Footnote 81 .
Using these 4 themes, we used an iterative process to bring together qualitative and quantitative methodological approaches through principles of intersectionality and social epidemiology to better understand and describe mental health inequalities in Canada. For a visual representation of how we used the qualitative literature to drive the thematic analysis and selection of quantitative trends refer to Figure 2.
Figure 2: A visual representation of the thematic analysis and selection of quantitative trends
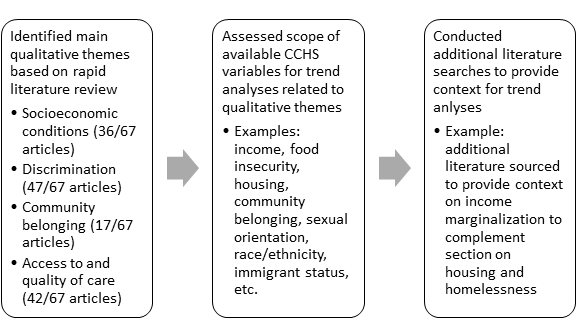
Figure 2: Text description
- Box 1 (Left): Identified main qualitative themes based on rapid literature
review
- This box lists the main qualitative themes that were identified from a rapid review of
67 articles. Each theme is accompanied by the number of articles in which it was
discussed:
- Socioeconomic conditions (37/67 articles)
- Discrimination (47/67 articles)
- Community belonging (17/67 articles)
- Access to and quality of care (42/67 articles)
- This box lists the main qualitative themes that were identified from a rapid review of
67 articles. Each theme is accompanied by the number of articles in which it was
discussed:
- Box 2 (Middle): Assessed scope of available CCHS variables for trend analyses
related to qualitative themes
- This box outlines the process of assessing the available variables in the Canadian
Community Health Survey (CCHS) that can be used for trend analyses aligned with the
qualitative themes identified in Box 1. Examples of these variables include:
- Income
- Food insecurity
- Housing
- Community belonging
- Sexual orientation
- Race/ethnicity
- Immigrant status, etc.
- This box outlines the process of assessing the available variables in the Canadian
Community Health Survey (CCHS) that can be used for trend analyses aligned with the
qualitative themes identified in Box 1. Examples of these variables include:
- Box 3 (Right): Conducted additional literature searches to provide context for
trend analyses
- This box describes the final step in the process, which involved conducting additional literature searches to enrich the context for the trend analyses. An example provided is the sourcing of literature on income marginalization to complement analyses focused on housing and homelessness.
3.3 Quantitative Research Component: Outcomes and Surveys
A trend analysis to assess mental health inequality over time used cross-sectional data from the Canadian Community Health Survey (CCHS) (details in Technical Notes at https://health-infobase.canada.ca/mental-health/inequalities/technical-notes.html ) . Unless otherwise indicated, trends are presented for the following time intervals: 2007 to 2010, 2011 to 2013, 2014 to 2016, 2017 to 2019, and 2020 to 2022 (the COVID-19 period). This is to ensure sufficiently large sample sizes when analysing data for subpopulations. In 2015, Statistics Canada revised the CCHS methodology, including the sampling frames, data collection approach, and questionnaire content. However, examination of yearly trends in mental health outcomes and social determinants did not reveal any major anomalies around this time.
We chose to use the CCHS rather than any other national survey because it includes several mental health outcomes and social determinants, has a large sample size, and questionnaire content has been largely consistent across annual cycles. However, people living on reserves and in other Indigenous settlements in the provinces and those living in the Quebec health regions of Nunavik and Terres-Cries-de-la-Baie James are not covered by the CCHS, limiting findings on First Nations living on reserves and Inuit in northern communities of Quebec that are part of Inuit Nunangat. Moreover, the survey asks respondents to self-identify as First Nations, Inuit, or Métis, which may not always conform to the criteria set out by each Nation or People. With financial support from PHAC, the First Nations Information Governance Centre (FNIGC) is producing a report that focuses on the mental wellness of First Nations Peoples living on reserve and in northern communities. This report will use data from the Regional Health Survey, the first and only national health survey of First Nations. The FNIGC report, which is anticipated to be released in 2025, will complement and expand on some of the findings in this current report.
The quantitative analyses in this report focus on 2 positive mental health outcomes: mean life satisfaction and high self-rated mental health Footnote 35 . These measures were selected using qualitative assessments that took into account indicators previously used by the HIRI, coverage across population groups that are important to health equity, and a balance between Western and distinctions-based Indigenous understandings of mental wellness. Outcomes were prioritized because of the increasing attention paid to strengths-based reporting models. Such models may, for example, represent topics for which inequalities are understudied, such as indicators for resilience. The focus then moves beyond the problems or deficits inherent in inequality monitoring, which can contribute to stigma Footnote 82 .
Further, selected outcomes are aligned with federal and international quality of life frameworks Footnote 83 Footnote 84 . Accordingly, the report does not represent an exhaustive measurement of positive mental health, but rather a summary of select key indicators.
The mean life satisfaction outcome is based on respondents’ rating of “satisfaction with life as a whole right now” on a scale of 0 to 10, where 0 represents “very dissatisfied” and 10 “very satisfied.” Life satisfaction analyses excluded data from the 2007 to 2008 survey wave as that wave used a different scale. High self-reported mental health is determined by respondents’ reporting of mental health as “excellent” or “very good” compared to the other options of “good,” “fair,” or “poor.”
Another mental health–related outcome analyzed was unmet need for mental health services, which represents the proportion of people who reported having mental health service needs that were partially met or not met at all versus fully met. This outcome was chosen because it aligned with the qualitative literature research findings. Data for the outcome were not collected consistently across CCHS waves, so data from the 2012 CCHS – Mental Health and the 2022 Mental Health and Access to Care Survey (MHACS) were used instead. Both surveys are nationally representative and are similar in design to the annual CCHS.
The Survey on COVID-19 and Mental Health (2020-2021) was utilized for an exclusive and focused analysis of the socioeconomic impacts of COVID-19 on mental health.
The social determinants of health explored in this report include relative household income, employment status, household food security, race/ethnicity, immigrant status, Indigenous identity, sexual orientation, sex/gender, and sense of community belonging. The same method of concurrence with the qualitative evidence was used to determine these social determinants of health.
Whenever possible, quantitative findings were disaggregated by sex/gender. The CCHS reported on respondents’ sex alone until 2019, when a separate variable capturing gender was introduced. In this report, as in the 2018 Key Health Inequalities in Canada: A National Portrait Footnote 85 , we use the sex variable because of its consistency in reporting on sex and/or gender across the years. The use of this variable is based on the assumption that health inequalities between males and females are often driven by the interconnectedness of biologically and socially determined constructs of gender.
Figures showing the quantitative analyses discussed are in accordance with the section’s subject matter. Further details on the mental health outcomes and social determinants of health are described in the Technical Notes ( https://health-infobase.canada.ca/mental-health/inequalities/technical-notes.html ) . Additional outcomes and social determinants were also analyzed and are available in the accompanying online data tool at https://health-infobase.canada.ca/mental-health/inequalities/data-tool.html (refer to Table 1 for a full list).
Table 1. List of Indicators Available in the Report’s Data Tool
| Outcomes (Indicators) |
|---|
| Access to a regular health care provider |
| Anxiety disorder diagnosis |
| Depression and anxiety symptoms |
| Excellent/very good self-rated mental health |
| Flourishing mental health |
| High life stress |
| Mean life satisfaction |
| Mood disorder diagnosis |
| Poor/fair self-rated mental health |
| Strong sense of community belonging |
| Suicidal attempt |
| Suicidal ideation |
| Suicide plan |
| Unmet need for mental health services |
Table 2. List of Stratifiers Available in the Report’s Data Tool
| Stratifiers (By sex/gender and ...) |
|---|
| Ability to speak official language by geography |
| Access to a health care provider |
| Age |
| Education |
| Employment status |
| First official language spoken by geography |
| Geography |
| Household food security |
| Household income |
| Housing tenure |
| Immigrant status |
| Immigrant status by cultural/racial background |
| Immigration recency |
| Indigenous identity – First Nations (off reserve), Inuit, and Métis |
| Living alone |
| Marital status |
| Multiple jobs |
| Neighbourhood immigration and visible minority concentration |
| Neighbourhood material resources index |
| Occupation |
| Occupational mismatch |
| Race/ethnicity |
| Rural/urban residence |
| Sense of community belonging |
| Sexual orientation |
3.3.1 Measuring Population Mental Health: Canada’s Approach to Surveillance
Gathering information about the mental health of the entire population is crucial for shaping mental health systems and services and fostering overall mental health. As more holistic understandings of mental health have emerged, Canadian mental health surveillance efforts have expanded the range of mental health indicators collected through national social and health surveys Footnote 52 to include measures of mental distress, which may not necessarily correspond with a diagnosis of a mental illness, and of positive mental health. Monitoring both dimensions of mental health, such as mental distress and positive mental health, is important to inform strategies that seek to identify risk and protective factors, such as economic status, community belonging, and social interactions (and inequalities within these) that can support mental health promotion efforts.
Canada has well-established systems for monitoring various states of mental illness, suicide, and positive mental health. The Positive Mental Health Surveillance Indicator Framework tracks a number of positive mental health outcomes, such as self-rated mental health, happiness, life satisfaction, and psychological and social well-being, and their associated risk and protective factors, primarily using data from national health surveys (for example the CCHS) Footnote 35 . The PHAC Suicide Surveillance Indicator Framework provides information on suicide and self-inflicted injury outcomes and their associated risk and protective factors.
The Canadian Chronic Disease Surveillance System (CCDSS) monitors indicators of mental illness using administrative data. These indicators include the use of health services for mental illness and alcohol- and drug-induced disorders, mood and anxiety disorders, and incidence and prevalence of and mortality from schizophrenia Footnote 86 . PHAC also monitors the prevalence of certain self-reported diagnoses of mental disorders using national surveys such as the CCHS Footnote 87 .
Finally, the HIRI provides comprehensive data on the distribution of positive and negative mental health status in different population groups according to a variety of socioeconomic determinants, which can be used to help advance health equity Footnote 88 .
3.4 Implications for This Report and Public Health Surveillance
To reflect the diversity of definitions and constructs described in Sections 2 and 3, this report and the accompanying online data tool explore social determinants of mental health and outcomes that span the dual continua of mental health, from indicators of positive mental health, such as high self-reported mental health and life satisfaction, to associated behaviours, such as substance use, and mood and anxiety disorder diagnoses and related morbidity.
Reflecting critically on how health outcomes are constructed and defined is a useful exercise for researchers devising Canadian public health surveillance systems. In the qualitative literature review, concepts and definitions of mental health varied widely between studies. While some studies referred to the WHO definition of health as a “state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity” Footnote 42 , participants in qualitative research studies rarely referred to any one definition. Instead, they spoke of “stress,” “anxiety,” “distress,” “hardship,” “suffering,” “struggling,” and “difficulty,” among other expressions. This raises questions about whether the mental health measures used in population health surveys are relevant and understood by all respondents. In Section 4 and the Discussion, we focus on people who understand and describe mental health in different ways and how mental health can be discussed more broadly.
4. Findings
4.1 Drivers of Mental Health Inequality in Canada
Using a narrative synthesis, we identified four themes related to the social determinants of mental health and well-being: socioeconomic conditions, racism and discrimination, social and cultural connection, support networks, and sense of community belonging, and access, use, and quality of health care services. We conducted a rapid review of 67 qualitative studies published between 2012 and 2022 that explored the social determinants of mental health and well -being in Canada (refer to the Technical Notes ( https://health-infobase.canada.ca/mental-health/inequalities/technical-notes.html ) for detailed methods). The reviewed qualitative research made explicit use of at least 12 theories and theoretical frameworks or models to explore and explain the systems, structures, and forces that shape the social conditions and inequalities in Canadian society. Among these are intersectionality theory; social ecological theory; critical feminist theory; risk environment frameworks; systemic, structural, and symbolic violence; hegemonic masculinity; employment strain model; minority stress theory; and the social determinants of health framework. Arguably, these theories all have the same main purpose of recognizing the relationship of power and privilege afforded to some rather than to others. Many of these theories provide well-supported explanations of the complex, interrelated, and multilevel processes that can result in mental health inequalities. Each explanation identifies unique structural drivers of inequality that occur at a societal level.
These theories recognize that: 1) multilevel processes shape the distribution of social conditions across society and hence the resulting health inequalities (i.e., from the individual, to interpersonal, community, and societal levels); 2) systems of power shape inequalities in health-determining social conditions; and 3) the need to focus on reducing health inequalities to improve the health status of subpopulations.
The mean life satisfaction outcome is based on CCHS respondents’ rating of “satisfaction with life as a whole right now” on a scale of 0 to 10, where 0 represents “very dissatisfied” and 10 “very satisfied.” The high self-reported mental health outcome is determined based on respondents’ reporting of mental health as “excellent” or “very good” compared to the other options of “good,” “fair,” or “poor.”
We recognize that the scope of our literature search may have influenced the types of studies included, and therefore these themes. To address this potential limitation, we conducted a supplementary search of systematic reviews of the social determinants of mental health inequalities to validate our themes (described in detail in Section 3.2.1).
In this section we demonstrate that positive mental health is not experienced equally by everyone in Canada. We profile inequalities at the population level based on 2 indicators—high self-reported mental health and mean life satisfaction—using data from annual cross-sectional components of the CCHS from 2007 to 2021 (refer to Section 3.3 or Technical Notes ( https://health-infobase.canada.ca/mental-health/inequalities/technical-notes.html ) for more details on the chosen indicators). Definitions adopted for indicators are in Section 3.3.
Positive mental health indicators are particularly important as a relationship has been established between high self-rated mental health and health care utilization Footnote 89 and of elevated risk of chronic disease and death Footnote 90 . In addition, recent studies of the mental health impacts of the COVID-19 pandemic have focused on a variety of positive mental health measures, including life satisfaction and self-perceived mental health Footnote 91 Footnote 92 Footnote 93 .
Positive mental health outcomes such as life satisfaction have been shown to vary across countries. In 2022, people living in Canada described their overall satisfaction with life as 7 on a scale of 0 to 10 (compared to the OECD average of 6.7). A few countries, for example, Denmark, Finland, Iceland, the Netherlands, and Switzerland, had average scores of 7.5 or higher Footnote 94 . At the other end of the scale, low levels of life satisfaction (a score of 4 or lower out of 10) were reported by 6.7% of the population in OECD countries from 2013 to 2020. In Canada, less than 3% of the population reported such low scores Footnote 95 . However, aggregate estimates at a country level do not capture within-country differences between populations groups nor widening or narrowing inequalities through time. Further, different social settings and cultural factors may influence different countries’ residents’ perceptions when grading their life satisfaction, hindering cross-country comparisons in many of the international reports.
Despite Canada’s relatively high level of overall positive mental health (as measured by life satisfaction), it is essential to examine within-country distributional differences (or inequalities). This is particularly important because post-pandemic recovery has raised the need to urgently address health inequalities that may have been exacerbated during and by the pandemic. In this section we provide a portrait of the distribution of positive mental health outcomes across different population groups and/or different determinants of health.
4.1.1 Socioeconomic Conditions: Impacts on Mental Health and Well-Being
Socioeconomic status is an important determinant of mental health across different life stages, in Canada and around the world Footnote 96 Footnote 97 Footnote 98 Footnote 99 . The association between socioeconomic status and mental health is influenced by factors that include lack of access to material and social resources and opportunities, stigma and discrimination, and social inequality Footnote 100 . This association is often described in terms of a dual cycle of financial insecurity and poor mental health (also referred to as a bidirectional relationship). That is, changes in income and material resources directly impacting mental health and conversely, how poor mental health might lead to worsening economic outcomes Footnote 100 Footnote 101 . This cycle can continue across generations. Breaking this cycle requires comprehensive approaches that simultaneously address the structural, systemic, and institutional causes of financial insecurity and an inequitable distribution of wealth as well as poor mental health Footnote 79 .
In this section, we describe changes in mental health inequalities over time related to the social determinants of health. These include socioeconomic position (for example, income level, employment status), daily living conditions (for example, stable and safe housing), and structural drivers (for example, food insecurity and working conditions). Findings also reflect mental health inequalities during, and prior to, the COVID-19 pandemic.
Income
Income, poverty, and material deprivation are linked to mental health, as is a person’s socioeconomic position in terms of their employment status or education, for example Footnote 97 Footnote 102 . Psychosocial stress theories posit that relative deprivation may provoke social comparison and contribute to the development of mental health problems by increasing chronic stress, social isolation, unhealthy behaviours, and low self-esteem Footnote 103 . Socioeconomic gradients in mental health—where outcomes tend to be worse among those with the lowest income, lower levels of educational attainment, and low-skilled occupations and improve gradually up the rungs of the socioeconomic ladder—are well documented in Canada Footnote 85 .
Figure 3.A and 3.B show income gradients in mean life satisfaction and high self-reported mental health prevalence over time among males and females. Income gradients narrowed over time, both before (2017–2019) and during the COVID-19 pandemic (2020 to 2022). In 2007 to 2010, there was an approximate 19 percentage-point difference in high self-rated mental health between those in the lowest and those in the highest income quintiles (19.2 for males and 18.7 for females). In 2014 to 2016, the percentage point difference peaked at 20.7 among males and 21.5 among females. By 2020 to 2022, inequalities had narrowed to 12.2 and 11.2 percentage points for males and females, respectively. Over time, income-related inequality in high self-rated mental health was largely similar among females and males.
For life satisfaction, the reduction in income-related inequality over time, which was more prominent among females than males, reflected both an increase in life satisfaction for those in the lowest income quintile and a decline for the more economically advantaged. The narrowing of absolute income-related inequality in high self-rated mental health over time primarily reflected steeper declines among people in higher income quintiles, especially since 2014 to 2016.
Figure 3.A Trends in mean life satisfaction by sex/gender and household income quintile, population aged 12 years and older, 2009–2022
| Year | Sex | Difference in mean life satisfaction score Lowest (Q1) vs. highest (Q5) income quintile (reference) |
Absolute change (95% CI) | Relative change |
|---|---|---|---|---|
| 2009-10 | Male | -0.84 (-0.92, -0.75) | -0.14 (-0.26, -0.02) | -17 |
| 2011-13 | Male | -0.97 (-1.05, -0.89) | ||
| 2014-16 | Male | -1.10 (-1.17, -1.02) | ||
| 2017-19 | Male | -0.84 (0.91, -0.78) | ||
| 2020-22 | Male | -0.70 (-0.78, -0.61) | ||
| 2009-10 | Female | -0.93 (-1.01, -0.85) | -0.40 (-0.51, -0.28) | -43 |
| 2011-13 | Female | -0.96 (-1.02, -0.89) | ||
| 2014-16 | Female | -1.07 (-1.14, -1.01) | ||
| 2017-19 | Female | -0.77 (-0.83, -0.70) | ||
| 2020-22 | Female | -0.53 (-0.61, -0.45) |
Abbreviations: CI, confidence interval; Q1, quintile 1 or the lowest income group; Q5, quintile 5 or the highest income group; SD, score difference; CCHS, Canadian Community Health Survey.
Notes:
Mean life satisfaction: reported level of satisfaction with life as a whole right now, on a scale of 0 to 10, where 0 means “very dissatisfied” and 10 means “very satisfied.” Negative values of the life satisfaction score differences (SDs) indicate absolute income-related inequalities in life satisfaction over the full time series. A value of 0 indicates that no difference exists between groups on that mental health outcome at a given time point. Changes in inequality are expressed in both absolute and relative scales between only the first and last time periods.
Absolute change calculation: (SD in 2009–2010)−(SD in 2020-2022).
Relative (%) change calculation: 100×[(SD in 2009-2010)−(SD in 2020-2022)/(SD in 2009-2010)].
Absolute and relative change interpretation: positive values indicate an increasing trend in income-related inequality in life satisfaction; negative values indicate a decreasing inequality trend.
Income quintiles are based on self-reported household income adjusted for household size, community size, and province of residence.
Data are from annual waves of the Canadian Community Health Survey (CCHS); population sample is aged 12+ years; estimates are age-standardized to the 2016 Census population using 5-year age intervals. Analyses excluded data from the 2007–2008 survey wave, which used a different life satisfaction scale. Caution is warranted when comparing estimates from cycles prior to 2015 and for data released 2022. We do not exclude the possibility that trends observed may have been influenced by different methodologies used in the CCHS, including a new sample design in 2015.
For more information on data and analysis considerations refer to https://health-infobase.canada.ca/mental-health/inequalities/technical-notes.html . Inequality trends for other mental health outcomes (e.g., suicidality, depressive symptomatology, life stress) are in the accompanying online data tool at https://health-infobase.canada.ca/mental-health/inequalities/data-tool.html .
Figure 3.B Trends in excellent/very good self-rated mental health by sex/gender and household income quintile, population aged 12 years and older, 2007–2022
| Year | Sex | Prevalence difference for excellent/very good self-rated mental health (95% CI) Lowest (Q1) vs. highest (Q5) income quintile (reference) |
Absolute change (95% CI) | Relative change |
|---|---|---|---|---|
| 2007-10 | Male | -19.2 (-20.7, -17.7) | -7.0 (-9.7, -4.2) | -36 |
| 2011-13 | Male | -20.3 (-22.3, -18.3) | ||
| 2014-16 | Male | -20.7 (-22.7, -18.7) | ||
| 2017-19 | Male | -17.3 (-19.1, -15.4) | ||
| 2020-22 | Male | -12.2 (-14.5, -9.9) | ||
| 2007-10 | Female | -18.7 (-20.2, -17.3) | -7.5 (-10.1, -4.9) | -40 |
| 2011-13 | Female | -19.4 (-21.2, -17.7) | ||
| 2014-16 | Female | -21.5 (-23.3, -19.8) | ||
| 2017-19 | Female | -16.0 (-17.8, -14.2) | ||
| 2020-22 | Female | -11.2 (-13.4, -9.1) |
Abbreviations: CI, confidence interval; PD, prevalence difference; Q1, quintile 1 or the lowest income group; Q5, quintile 5 or the highest income group; SRMH, self-rated mental health, vs., versus; CCHS, Canadian Community Health Survey
Notes:
Excellent/very good self-rated mental health (SRMH): percent of the population who reported their mental health as “excellent” or “very good” (vs. “good” or “fair” or “poor”). Negative values of the Q1 vs. Q5 prevalence difference (PD) indicate absolute income-related inequalities in excellent/very good SRMH over the full time series. A value of 0 indicates that no difference exists between groups on that mental health outcome at a given time point. Changes in inequality are expressed in both absolute and relative scales between only the first and last time periods.
Absolute change calculation: (PD in 2007–2010)−(PD in 2020-2022).
Relative (%) change calculation: 100×[(PD in 2007–2010)−(PD in 2020-2022)]/(PD in 2007–2010)].
Absolute and relative change interpretation: positive values indicate an increasing trend in income-related inequality in excellent/very good SRMH, negative values indicate a declining inequality trend.
Income quintiles are based on self-reported household income adjusted for household size, community size, and province of residence.
Data are from annual waves of the Canadian Community Health Survey; population sample is aged 12+ years; estimates are age-standardized to the 2016 Census population using 5-year age intervals. Caution is warranted when comparing estimates from cycles prior to 2015 and for data released 2022. We do not exclude the possibility that trends observed may have been influenced by different methodologies used in the CCHS, including a new sample design in 2015.
For more information on data and analysis considerations refer to https://health-infobase.canada.ca/mental-health/inequalities/technical-notes.html . Inequality trends for other mental health outcomes (e.g., suicidality, depressive symptomatology, life stress) are in the accompanying online data tool at https://health-infobase.canada.ca/mental-health/inequalities/data-tool.html .
Food Insecurity
According to Health Canada, food insecurity is “the inability to acquire or consume an adequate diet quality or sufficient quantity of food in socially acceptable ways, or the uncertainty that one will be able to do so” Footnote 328 . Household food insecurity is a marker of material deprivation Footnote 328 .
Food insecurity, defined as inadequate or insecure access to food due to financial constraints, affected approximately 6.9 million Canadians in 2021 Footnote 104 . Figures 4.A and 4.B show clear gradients in mean life satisfaction and high self-rated mental health, and over time, according to level of food security (secure, moderately insecure, severely insecure). During the COVID-19 pandemic (2020–2022), the prevalence of high self-rated mental health was approximately 32 percentage points lower among males experiencing severe food insecurity than among males who were food secure; for females, the difference was 36 percentage points. This is consistent with current evidence linking food insecurity to poor mental health in Canada Footnote 105 Footnote 106 Footnote 107 .
Food security–related gaps in life satisfaction and high self-rated mental health tended be consistent over time (Figures 4.A and 4.B). The exception was an approximately 5 percentage-point increase in the gap in high self-rated mental health for females experiencing severe food insecurity compared to those who were food secure. This corresponded to an 15% increase in relative inequality between the 2007 to 2010 and 2020 to 2022.
Figure 4.A Trends in mean life satisfaction by sex/gender and level of household food insecurity, population aged 12 years and older, 2009–2022
| Year | Sex | Group | Difference in mean life satisfaction score (95% CI) | Absolute change (95% CI) | Relative change |
|---|---|---|---|---|---|
| 2009-22 | Male | Food secure (reference) | 0 | - | - |
| 2009-10 | Male | Moderately food insecure | -1.09 (-1.24, -0.95) | -0.007 (-0.27, 0.13) | -6 |
| 2011-13 | Male | Moderately food insecure | -1.11 (-1.32, -0.89) | ||
| 2014-16 | Male | Moderately food insecure | -1.18 (-1.33, -1.03) | ||
| 2017-19 | Male | Moderately food insecure | -0.97 (-1.10, -0.85) | ||
| 2020-22 | Male | Moderately food insecure | -1.02 (-1.15, -0.89) | ||
| 2009-10 | Male | Severely food insecure | -1.83 (-2.17, -1.49) | 0.12 (-0.29, 0.53) | 7 |
| 2011-13 | Male | Severely food insecure | -2.02 (-2.27, -1.77) | ||
| 2014-16 | Male | Severely food insecure | -1.90 (-2.19, -1.61) | ||
| 2017-19 | Male | Severely food insecure | -1.94 (-2.12, -1.77) | ||
| 2020-22 | Male | Severely food insecure | -1.95 (-2.18, -1.72) | ||
| 2009-22 | Female | Food secure (reference) | 0 | - | - |
| 2009-10 | Female | Moderately food insecure | -0.93 (-1.06, -0.80) | 0.08 (-0.09, 0.26) | 9 |
| 2011-13 | Female | Moderately food insecure | -1.04 (-1.15, -0.93) | ||
| 2014-16 | Female | Moderately food insecure | -1.02 (-1.15, -0.88) | ||
| 2017-19 | Female | Moderately food insecure | -0.97 (-1.08, -0.87) | ||
| 2020-22 | Female | Moderately food insecure | -1.01 (-1.13, -0.90) | ||
| 2009-10 | Female | Severely food insecure | -1.69 (-1.93, -1.44) | 0.08 (-0.22, 0.38) | 5 |
| 2011-13 | Female | Severely food insecure | -1.78 (-2.02, -1.55) | ||
| 2014-16 | Female | Severely food insecure | -1.74 (-1.92, -1.56) | ||
| 2017-19 | Female | Severely food insecure | -1.87 (-2.02, -1.71) | ||
| 2020-22 | Female | Severely food insecure | -1.76 (-1.95, -1.58) |
Abbreviations: CI, confidence interval; SD, score difference; CCHS, Canadian Community Health Survey.
Notes:
Mean life satisfaction: reported level of satisfaction with life as a whole right now, on a scale of 0 to 10, where 0 means “very dissatisfied” and 10 means “very satisfied.” Negative values of the life satisfaction score differences (SDs) indicate absolute food security–related inequality in life satisfaction over the full time series. A value of 0 indicates that no difference exists between groups on that mental health outcome at a given time point. Changes in inequality are expressed in both absolute and relative scales between only the first and last time periods.
Absolute change calculation: (SD in 2009–2010)–(SD in 2020–2022).
Relative (%) change calculation: 100×[(SD in 2009–2010)−(SD in 2020–2022)/(SD in 2009–2010)].
Absolute and relative change interpretation: positive values indicate an increasing trend in food security–related inequality in life satisfaction; negative values indicate a decreasing inequality trend.
Food security status was determined from a set of 18 questions describing food access, quality, and intake in the previous 12 months.
Data are from annual waves of the Canadian Community Health Survey; population sample is aged 12+ years; estimates are age-standardized using 2016 Census 5-year age intervals. Analyses exclude 2007–2008 data, as that survey wave used a different life satisfaction scale. Caution is warranted when comparing estimates from cycles prior to 2015 and for data released 2022. We do not exclude the possibility that trends observed may have been influenced by different methodologies used in the CCHS, including a new sample design in 2015.
For more information on data and analysis considerations refer to https://health-infobase.canada.ca/mental-health/inequalities/technical-notes.html . Inequality trends for other mental health outcomes (e.g., suicidality, depressive symptomatology, life stress) by level of food security are shown in the accompanying online data tool at https://health-infobase.canada.ca/mental-health/inequalities/data-tool.html .
Figure 4.B Trends in excellent/very good self-rated mental health by sex/gender and level of household food insecurity, population aged 12 years and older, 2007–2022
| Year | Sex | Group | Prevalence difference for excellent/very good self-rated mental health (95% CI) | Absolute change (95% CI) | Relative change |
|---|---|---|---|---|---|
| 2007-22 | Male | Food secure (reference) | 0 | - | - |
| 2007-10 | Male | Moderately food insecure | -21.6 (-24.4, -18.7) | -0.5 (-4.8, 3.7) | -3 |
| 2011-13 | Male | Moderately food insecure | -22.2 (-25.7, -18.6) | ||
| 2014-16 | Male | Moderately food insecure | -23.2 (-26.8, -19.6) | ||
| 2017-19 | Male | Moderately food insecure | -20.6 (-23.6, -17.7) | ||
| 2020-22 | Male | Moderately food insecure | -21.0 (-24.2, -17.9) | ||
| 2007-10 | Male | Severely food insecure | -32.1 (-36.7, -27.5) | 0.2 (-6.0, 6.4) | 1 |
| 2011-13 | Male | Severely food insecure | -29.7 (-34.8, -24.6) | ||
| 2014-16 | Male | Severely food insecure | -34.3 (-38.5, -30.1) | ||
| 2017-19 | Male | Severely food insecure | -33.8 (-38.3, -29.2) | ||
| 2020-22 | Male | Severely food insecure | -32.2 (-36.4, -28.1) | ||
| 2007-22 | Female | Food secure (reference) | 0 | - | - |
| 2007-10 | Female | Moderately food insecure | -20.9 (-23, -18.7) | -2.5 (-6.1, 1.2) | -12 |
| 2011-13 | Female | Moderately food insecure | -18.9 (-21.9, -15.9) | ||
| 2014-16 | Female | Moderately food insecure | -24.6 (-27.8, -21.4) | ||
| 2017-19 | Female | Moderately food insecure | -19.2 (-21.6, -16.7) | ||
| 2020-22 | Female | Moderately food insecure | -18.4 (-21.3, -15.5) | ||
| 2007-10 | Female | Severely food insecure | -31.1 (-34.6, -27.7) | 4.6 (0.1, 9.0) | 15 |
| 2011-13 | Female | Severely food insecure | -29.7 (-34.9, -24.6) | ||
| 2014-16 | Female | Severely food insecure | -30.6 (-34.7, -26.4) | ||
| 2017-19 | Female | Severely food insecure | -36.8 (-39.8, -33.8) | ||
| 2020-22 | Female | Severely food insecure | -35.7 (-38.5, -32.9) |
Abbreviations: CI, confidence interval; PD, prevalence difference; SRMH, self-rated mental health; CCHS, the Canadian Community Health Survey.
Notes:
Excellent/very good self-rated mental health: percent of the population who reported their mental health as “excellent” or “very good” (vs. “good” or “fair” or “poor”). Negative values of the food insecure vs. food secure prevalence differences (PDs) indicate absolute inequality in excellent/very good self-rated mental health (SRMH) over the full time series. A value of 0 indicates that no difference exists between groups on that mental health outcome at a given time point. Changes in inequality are expressed in both absolute and relative scales between only the first and last time periods.
Absolute change calculation: (PD in 2007–2010)−(PD in 2020-2022).
Relative (%) change calculation: 100×[(PD in 2020-2022)−(PD in 2007–2010)/(PD in 2007–2010).
Absolute and relative (%) change interpretation: positive values indicate an increasing trend in food security–related inequality in excellent/very good SRMH, and negative values indicate a declining inequality trend.
Food security status was determined from a set of 18 questions describing food access, quality, and intake in the previous 12 months.
Data are from annual waves of the Canadian Community Health Survey; population sample is aged 12+ years; estimates are age-standardized using 2016 Census 5-year age intervals. Caution is warranted when comparing estimates from cycles prior to 2015 and for data released 2022. We do not exclude the possibility that trends observed may have been influenced by different methodologies used in the CCHS, including a new sample design in 2015.
For more information on data and analysis considerations refer to https://health-infobase.canada.ca/mental-health/inequalities/technical-notes.html . Inequality trends for other mental health outcomes (e.g., suicidality, depressive symptomatology, life stress) by level of food security are shown in the accompanying online data tool at https://health-infobase.canada.ca/mental-health/inequalities/data-tool.html .
Safe and Stable Housing
Housing is recognized as a human right under the National Housing Strategy Act Footnote 108 . In 2021, 1 in 10 households in Canada lived in core housing need, that is, the households (made up of families or groups) did not have affordable, adequate, or suitable housing Footnote 109 . Canada’s housing situation is particularly pressing in major urban centres, where high housing costs and limited stock of affordable dwellings have made it difficult for many people to secure safe and stable housing. This is especially problematic for those living at low income, receiving social assistance, or those requiring supportive or transitional housing.
Numerous studies have shown that inadequate or unaffordable housing can contribute to many mental health problems, including anxiety, depression, and stress Footnote 110 Footnote 111 . For instance, in Canada, individuals living with a mental health–related disability (defined as experiencing limitations in their daily activities because of difficulties with an emotional, psychological, or mental health condition) are more than twice as likely as those without such a disability to be in core housing need in 2017 Footnote 112 .
Homelessness appears to be increasing across Canada, particularly among younger people Footnote 113 Footnote 114 . Adequate housing provides a sense of stability and is connected to feelings of self-worth and increased quality of life Footnote 115 . Conversely, being unhoused and having to rely on shelters is associated with feelings of worthlessness, hopelessness, disappointment, and negative self-esteem Footnote 116 . Housing instability intersects with poverty and unemployment Footnote 116 . In addition, experiences of violence, encounters with the criminal justice system, and challenges with immigration experienced by those living with housing instability compound feelings of powerlessness, discrimination, and social disconnect, all of which that negatively impact mental health Footnote 116 .
While shelters offer some respite by providing temporary housing, numerous issues related to the quality and safety of spaces affect mental health. These include social restrictions that impact an individual’s ability to maintain contact with family and friends, aggression, threats of assault, and exposure to sexual acts Footnote 115 .
Unhoused women are often overlooked at the policy level, to the point that they have been described as the “invisible homeless” Footnote 111 . Women often rely on informal housing measures—staying with friends, family, and in many cases, with unknown men, putting themselves at risk for sexual violence Footnote 111 . The lack of safe shelter spaces contributes to feelings of stress, vulnerability, and powerlessness and worse mental health outcomes Footnote 111 .
Among individuals with severe mental illness, shelter spaces are more frequently accessed by men than by women. For women with severe mental illness who reside in rural areas, the lack of safe and supportive housing might necessitate relocating to urban centres to access more appropriate shelter space. One service provider described the experiences of women with severe mental illness as follows:
Women’s [with severe mental illness] homelessness tends to be a little bit more invisible. We certainly have a number of women who have lived with their sister for a long time or crashed with unsavoury males over a series of years. They have, in fact, been homeless—they have just been temporarily couched. If you look at resource availability … they operate out of men’s shelters, and aren’t always in a safe environment for women. [Resources] certainly seem to be centred on male-accessible places … all these guys have all these shelters to choose from and if they get booted out of one after 4 weeks they just move over to the next one. We turn hundreds and hundreds of women away from our shelter because we just don’t have the beds. Footnote 111
Men with severe mental illness report living in substandard provisional housing or being forced to live in “drug-infested” areas where public drug use is common. Living in such areas increases anxiety and increases risk of relapse among men and women alike Footnote 111 . Men also have more difficulty than women accessing suitable housing if they have a child. Women sometimes have improved access to housing because gender stereotypes and gender roles cast them as “child bearers” and “requiring family housing” Footnote 111 . Conversely, women have described avoiding mental health care because they feared that if authorities learned about their mental illness, their child would be taken into custody and that their illness would prevent them from ever regaining custody. There were also instances where male children were not allowed in housing for females. Footnote 111 .
Individuals in shelters experienced discrimination based on sex/gender and race or ethnicity. For example, a woman wearing a hijab stood out based on her appearance Footnote 111 .
Indigenous women with severe mental illnesses who live in rural areas and northern communities also experienced housing challenges. Non-Indigenous men have significantly more power than Indigenous women, as highlighted by a service provider’s description:
We worked with a woman from a small Aboriginal community. Her non-Aboriginal husband got on the housing authority board and illegally had her name removed from home ownership papers just because the government could. … so in small communities it is very controlled by men and they will choose men over Aboriginal women.… Aboriginal women are the most marginalized Footnote 111 .
The intersection of geographic location, sexism, racism, and intergenerational trauma has led to situations where women have little to no control over their housing status and few options to leave their towns if structural barriers have affected access to transportation.
Box 4.1: Housing and First Nations off-reserve, Inuit, and Métis
First Nations, Inuit, and Métis in Canada consistently experience worse housing conditions than their non-Indigenous counterparts. The 2021 Census found that 17.1% of Indigenous People (21.4% of First Nations, 7.9% of Métis, and 40.1% of Inuit) lived in overcrowded housing considered unsuitable for the number of occupants Footnote 117 . In addition, compared to their non-Indigenous counterparts, Indigenous People were almost twice as likely to live in crowded housing and almost 3 times as likely to live in a dwelling in need of major repairs (16.4% of Indigenous Peoples, among them 19.7% of First Nations, 10% of Métis, and 26.2% of Inuit, compared to 5.7% for non-Indigenous People) Footnote 117 . Indigenous People who reported living in a dwelling that needed major repairs were significantly more likely than those whose homes needed only minor or no repairs to report fair or poor self-rated mental health Footnote 118 .
These disparities are the result of, and maintained by, a legacy of colonialism that perpetuate systemic and structural barriers for Indigenous Peoples. Some of the barriers include racial profiling and discrimination by landlords, employers, police, and social service agencies Footnote 119 :
I tried to get a place in the suburbs. I thought I had an appointment and there was a vacancy sign, but when I showed up they told me it was rented Footnote 119 .
Discrimination often begins when the landlord hears your accent, or they see your face, and they know you are Aboriginal.… There are some slum landlords who take advantage of tenants Footnote 119 .
Housing tends to be viewed as part of a continuum in which homeownership is held as the ideal Footnote 120 . Housing tenure impacts mental health through a variety of mechanisms. Home ownership may lead to an increase in sense of self-esteem and prestige; however, it also comes with the potential for the stress and anxiety associated with financial strain as a result of servicing mortgage debt. On the other hand, rental instability can lead to challenges accessing and maintaining social assistance networks that support mental wellness Footnote 121 .
We used Canadian Community Health Survey (CCHS) data to examine inequalities in life satisfaction for the intersection of Indigenous identity and housing tenure from 2009 and 2022. It should be noted that the CCHS has no clear-cut indicator of housing insecurity, thus housing tenure was utilized instead given its availability in the CCHS and similarity to the concepts of housing insecurity and stability Footnote 122 Footnote 123 . In addition, the CCHS does not survey people living on reserve where housing conditions have been reported to be worse than off reserve (that is, too small for the number of occupants, resulting in overcrowding, and in need of major repairs) Footnote 117 . For further disaggregation of findings by sex, refer to the accompanying online data tool at https://health-infobase.canada.ca/mental-health/inequalities/data-tool.html .
Findings show that life satisfaction is often significantly higher among homeowners regardless of Indigenous identity. Between 2009-2010 and 2020-2022, First Nations living off reserve and Métis homeowners reported similar levels of life satisfaction compared to non-Indigenous homeowners. However, the gap in life satisfaction between First Nations living off reserve and Métis people who rent and non-Indigenous renters was consistently more pronounced. Inuit renters and homeowners showed similar levels of life satisfaction in later years.
Employment, Work Conditions, and Mental Health and Well-Being
Employment overall has a positive impact on mental health, providing money, resources, a sense of purpose and identity, as well as opportunities to develop skills, self-esteem, and social connections Footnote 124 . Becoming or being unemployed can result in loss of income and benefits, which can affect standard of living, increase experiences of poverty, stigma, and shame, and cause a loss of daily structure and access to social contacts that can be particularly harmful to mental health. Unemployment is consistently associated with lower psychological well-being and increased risk of depression, anxiety, and suicidal behaviour Footnote 125 Footnote 126 . These associations are bidirectional—unemployment can worsen a person’s mental health, and mental health issues can reduce a person’s ability to obtain and/or maintain a job Footnote 100 .
Studies that examined mental health at the intersection of sex/gender and unemployment have shown mixed results, although a majority suggests that unemployment may have greater mental health consequences for men Footnote 127 . Figures 5.A and 5.B show that, over time, employed individuals reported higher levels of life satisfaction as well as better levels of high self-reported mental health than their unemployed counterparts. With time, the unemployed–employed gap in life satisfaction increased for males and decreased for females. There was also evidence of increasing employment-related inequality in high self-reported mental health among males, with unemployed males reporting decreases in high self-report mental health between 2007–2010 and 2020–2022.
Figure 5.A. Trends in mean life satisfaction by sex/gender and employment status, population aged 18–75 years, 2009–2022
| Year | Sex | Difference in mean life satisfaction score Unemployed vs. employed (reference) |
Absolute change (95% CI) | Relative change |
|---|---|---|---|---|
| 2009-10 | Male | -0.48 (-0.56, -0.41) | 0.21 (0.09, 0.33) | 42 |
| 2011-13 | Male | -0.60 (-0.66, -0.54) | ||
| 2014-16 | Male | -0.78 (-0.85, -0.70) | ||
| 2017-19 | Male | -0.72 (-0.79, -0.64) | ||
| 2020-22 | Male | -0.69 (-0.78, -0.60) | ||
| 2009-10 | Female | -0.26 (-0.32, -0.19) | 0.00 (-0.09, 0.10) | 1 |
| 2011-13 | Female | -0.31 (-0.36, -0.26) | ||
| 2014-16 | Female | -0.36 (-0.41, -0.31) | ||
| 2017-19 | Female | -0.42 (-0.48, -0.35) | ||
| 2020-22 | Female | -0.26 (-0.33, -0.19) |
Abbreviations: CI, confidence interval; SD, score difference; CCHS, Canadian Community Health Survey.
Notes:
Mean life satisfaction: reported level of satisfaction with life as a whole right now, on a scale of 0 to 10, where 0 means “very dissatisfied” and 10 means “very satisfied.”. Negative values of the life satisfaction score differences (SDs) indicate absolute employment-related inequality in life satisfaction over the full time series. A value of 0 indicates that no difference exists between groups on that mental health outcome at a given time point. Changes in inequality are expressed in both absolute and relative scales between only the first and last time periods.
Absolute change calculation: (SD in 2009–2010)−(SD in 2020–2022).
Relative (%) change calculation: 100×[(SD in 2009–2010)−(SD in 2020–2022)/(SD in 2009–2010)].
Absolute and relative change interpretation: positive values indicate an increasing trend in employment-related inequality in life satisfaction; negative values indicate a decreasing inequality.
Data are from annual waves of the Canadian Community Health Survey; population sample is aged 18-75 years; estimates are age-standardized using 2016 Census 5-year age intervals. Analyses excluded data from the 2007–2008 survey wave, which used a different life satisfaction scale. Caution is warranted when comparing estimates from cycles prior to 2015 and for data released 2022. We do not exclude the possibility that trends observed may have been influenced by different methodologies used in the CCHS, including a new sample design in 2015.
For more information on data and analysis considerations refer to https://health-infobase.canada.ca/mental-health/inequalities/technical-notes.html . Inequality trends for other mental health outcomes (e.g., suicidality, depressive symptomatology, life stress) by level of food security are shown in the accompanying online data tool at https://health-infobase.canada.ca/mental-health/inequalities/data-tool.html .
Figure 5.B. Trends in excellent/very good self-rated mental health by sex/gender and employment status, population aged 18–75 years, 2007–2022
| Year | Gender | Prevalence difference for excellent/very good self-rated mental health (95% CI) Unemployed vs. employed (reference) |
Absolute change (95% CI) | Relative change |
|---|---|---|---|---|
| 2007-10 | Male | -11.7 (-13.0, -10.5) | 2.4 (-0.4, 5.1) | 20 |
| 2011-13 | Male | -13.2 (-14.8, -11.6) | ||
| 2014-16 | Male | -15.2 (-17, -13.5) | ||
| 2017-19 | Male | -15.8 (-17.5, -14.0) | ||
| 2020-22 | Male | -14.1 (-16.5, -11.7) | ||
| 2007-10 | Female | -8.6 (-9.7, -7.5) | -2.5 (-4.6, -0.4) | -29 |
| 2011-13 | Female | -10.6 (-11.9, -9.2) | ||
| 2014-16 | Female | -10.4 (-11.9, -8.9) | ||
| 2017-19 | Female | -10.2 (-11.7, -8.8) | ||
| 2020-22 | Female | -6.1 (-7.9, -4.2) |
Abbreviations: CI, confidence interval; PD, prevalence difference; SRMH, self-rated mental health; CCHS, Canadian Community Health Survey.
Notes:
Excellent/very good self-rated mental health (SRMH): percent of the population who reported their mental health as “excellent” or “very good” (vs. “good” or “fair” or “poor”). Negative values of the unemployed vs. employed prevalence differences (PDs) indicate absolute employment-related inequality in SRMH over the full time series. A value of 0 indicates that no difference exists between groups on that mental health outcome at a given time point. Changes in inequality are expressed in both absolute and relative scales between only the first and last time periods.
Absolute change calculation: (PD in 2007–2010)−(PD in 2020-2022).
Relative (%) change calculation: 100×[(PD in 2007–2010)−(PD in 2020-2022)/(PD in 2007–2010)].
Absolute and relative (%) change interpretation: positive values indicate an increasing trend in employment-related inequality in excellent/very good SRMH, and negative values indicate a decreasing inequality trend.
Employment status was determined based on respondents reporting working at a job or business the previous week (“yes” vs. “no”).
Data are from annual waves of the Canadian Community Health Survey ; population sample is aged 18–75 years; estimates are age-standardized using 2016 Census 5-year age intervals. Caution is warranted when comparing estimates from cycles prior to 2015 and for data released 2022. We do not exclude the possibility that trends observed may have been influenced by different methodologies used in the CCHS, including a new sample design in 2015.
For more information on data and analysis considerations refer to https://health-infobase.canada.ca/mental-health/inequalities/technical-notes.html . Inequality trends for other mental health outcomes (e.g., suicidality, depressive symptomatology, life stress) are shown in the accompanying online data tool at https://health-infobase.canada.ca/mental-health/inequalities/data-tool.html .
Employment Conditions
Employment is typically beneficial for mental health; however, access to suitable employment and working conditions also have a profound effect on psychological well-being. Occupation type and poor work conditions, including job insecurity, precarious employment, inadequate pay, excessive workload, difficult work hours, lack of benefits, harassment, and discrimination, are major causes of work-related stress and associated mental health problems and have impacts on families and communities Footnote 128 Footnote 129 Footnote 130 .
In Canada, unemployment and poor-quality employment and work conditions are disproportionately experienced by young people, those with lower educational attainment, and individuals and communities living in historically underserved conditions, including Indigenous, Black, and racialized people and immigrants Footnote 131 .
Newcomers to Canada often face employment-related challenges, including lack of recognition of foreign educational credentials, being overqualified for positions, difficulty acquiring requisite Canadian experience, challenges related to language competency, limited access to social and professional networks, and employer bias against hiring immigrants Footnote 132 . These challenges are also more likely to occur when recent immigrants are racialized Footnote 132 . Box 4.2 highlights qualitative data insights about the relationship between work conditions, immigrant status, and mental health Footnote 133 .
Box 4.2: Qualitative data insights: Work conditions, immigrant status, and mental health
Underlying structural barriers related to the intersections of gender, racialization, and immigrant status often impact access to meaningful employment that is commensurate with educational background and professional experience. Qualitative studies of immigrant populations in Canada note that many new immigrants, particularly those who are racialized, accept low-skill, low-wage, and insecure employment that does not match their educational credentials or employment experience for purposes of economic survival Footnote 133 Footnote 134 Footnote 135 Footnote 136 . This type of employment often has neither benefits nor long-term stability, leading to financial insecurity and inability to take time off to engage in health-seeking behaviours.
A female participant in one of the studies exploring the pathways between under- or unemployment and health in Canada Footnote 133 described the situation as follows:
When [immigrants] come here they don’t get proper jobs [to match] their skills … the jobs are often mismatched. So to support their family they try to do something that does not fit physically, mentally, or by skill set. Then what happens? Lots of injuries happen, and they become sick, emotionally they break down … and they feel very low. Footnote 133
Several forces perpetuate immigration, racial, or ethnic inequalities in occupational mismatch and deskilling. Some are technical and structural in nature, such as the decentralized, competitive, and expensive accreditation systems across Canadian provinces and territories; newcomers’ challenges with the English or French official languages; employers’ biases against foreign degrees; employers’ requirements for Canadian experience in order to enter the labour market; and employers’ reluctance to recognize professional work experience from other countries Footnote 137 Footnote 138 . Other forces are shaped by structural and systemic racism Footnote 134 , for example, bias against foreign accents Footnote 139 and against education, training, and accreditation from low- and middle-income countries Footnote 140 . The bias that training and knowledge capacity from lower-income countries is “deficient, incompatible, and inferior, hence invalid” has been attributed to systemic racism and discrimination Footnote 141 .
Canadian studies have documented the negative psychosocial impacts of occupational mismatch and deskilling Footnote 133 Footnote 134 Footnote 135 Footnote 141 , particularly when associated with precarious work conditions and financial hardships Footnote 133 Footnote 134 Footnote 135 , that result in feelings of disappointment, personal inadequacy or low self-esteem, distress, frustration, sadness, isolation, stress, fear, and anger Footnote 133 , and affecting overall well-being and life satisfaction. In a study of under/unemployment and health among immigrant women, one participant described her experience of occupational mismatch as follows:
I was a manager. I start work in a [coffee shop] and all the time I get very upset about the work [crying]. I talk to you very lightly, but from the bottom of my heart I really suffered a lot. I did. I did. Sometimes I was almost having—like not depression but thinking of suicide … I was thinking that on coming to Canada, [because] I speak English, I have good experience in USA, I should get at least an office job at $11 [per hour], but this didn’t happen for 8 years. So though I talk to you like it was nothing, I really feel very, very sad [crying]. Footnote 133
Women—and particularly racialized, immigrant women—face additional challenges that pertain to systemic gender norms and intersecting racial and gender-based discrimination. Racialized immigrant women are often relegated to nonregulated, parttime, and care-related work that is associated with lower pay. One study participant recounted her experience of intersecting gender and racial or ethnic discrimination:
I remember when I was asking someone from the bank, “How did you apply,” because I knew that she was also an immigrant, and she was saying that, “Oh, you’re better in the care-giving profession because you’re Filipino.” I was like, “Okay, so you’re labelling me that I cannot work in this kind of field” Footnote 133 .
Quantitative Analysis insights: Inequalities in Employment Overqualification by Intersections of Race and Immigrant Status
Using data from the CCHS, we assessed the prevalence of “overqualified” employment (also referred to as occupational mismatch or occupation mismatch). That is, people with university degrees working in National Occupational Classification (NOC) skill level categories C or D, where the job usually requires, at most, secondary school qualifications and/or on-the-job training. NOC is the national system for characterizing occupations in Canada, and it is subject to revisions and updates to reflect occupational changes over time Footnote 142 . Overall, racialized adult immigrants to Canada reported a higher prevalence of “overqualified” employment status (12% prevalence in 2020-2022) compared to White adult immigrants (6% in 2020-2022) and White adult non-immigrants (4% in 2020-2022). This pattern remained consistent before (2007-2010 to 2017-2019) and during the COVID-19 pandemic (2020–2022) and the gap seemed to widen over time.
For detailed information about the methodology, please refer to Technical Notes ( https://health-infobase.canada.ca/mental-health/inequalities/technical-notes.html ). For the full set of results and visualizations, refer to the accompanying online data tool tab at https://health-infobase.canada.ca/mental-health/inequalities/data-tool.html .
The COVID-19 Pandemic and Effects on Mental Health
In early 2020, public health measures, labour force changes, and international responses to contain the COVID-19 pandemic led to job losses or reduced work hours for more than 3 million Canadians, with young people aged 15 to 24 years, low-wage workers, 2SLGBTQI+ individuals, racialized and particularly Black people, and immigrants disproportionately affected Footnote 143 Footnote 144 Footnote 145 . Economic recessions and other events that reduce employment opportunities have in the past led to an increase in mental health problems and suicide mortality, especially among socioeconomically disadvantaged populations Footnote 146 Footnote 147 . A growing body of evidence suggests that a variety of mental health outcomes, including major depressive disorder, depressive symptoms, and self-rated mental health worsened during the COVID-19 pandemic Footnote 125 Footnote 148 Footnote 149 Footnote 150 . Occupational and financial disruptions, in addition to the profound social implications of quarantine and other public health measures, are presumed to have contributed to these declines in mental health Footnote 151 .
We used data from the Survey on COVID-19 and Mental Health to focus on the pronounced socioeconomic impacts on mental health — specifically, symptoms of depression and anxiety— during the COVID-19 pandemic. Prevalence rates of moderate/severe symptoms of depression and anxiety by job loss and financial difficulties are shown in Figure 5.C. Overall, compared to males, females experienced greater prevalence of symptoms of depression and anxiety during the pandemic; however, financial difficulties and job loss disproportionately affected the mental health of men. The prevalence of moderate/severe anxiety symptoms was 2.2 times higher among males and 1.5 times higher among females who reported job loss due to COVID-19 than among males and females who reported no job loss. This is consistent with evidence that the mental health consequences of major economic and labour force disruptions are often worse for socioeconomically disadvantaged males Footnote 152 .
Figure 5.C: Prevalence of moderate/severe symptoms of depression and anxiety by experiences of financial difficulties and job loss during the COVID-19 pandemic, by sex/gender, 2020–2021
|
Sex |
Comparison of moderate/severe depressive symptoms (%) by reported financial difficulties ( Reference = no financial difficulties ) |
Comparison of moderate/severe anxiety symptoms (%) by reported job loss ( Reference = no job loss ) |
||
|
Prevalence difference |
Prevalence ratio |
Prevalence difference |
Prevalence ratio |
|
|
Males |
19.4 (15.3, 23.5) |
2.9 (2.4, 3.4) |
10.1 (7.0, 13.2) |
2.2 (1.7, 2.7) |
|
Females |
21.4 (17.3, 25.5) |
2.3 (2.0, 2.5) |
7.2 (4.1, 10.3) |
1.5 (1.2, 1.7) |
Notes:
The severity of anxiety and depression were measured using the Generalized Anxiety Disorder Scale (GAD-7) and Patient Health Questionnaire (PHQ-9), respectively. These clinical screening tools are widely used in population health surveys to identify those who may have generalized anxiety disorder and major depressive disorder, with scores of 10 or greater (i.e., moderate to severe symptoms) in the 2 weeks prior to completing the survey. The data shown do not necessarily reflect a clinical diagnosis of these conditions.
Data are from the Statistics Canada Survey on COVID-19 and Mental Health (2020–2021). Population age 18+ years; estimates are age-standardized using 2016 Census 5-year age groups.
4.1.2 The Impacts on Mental Health of Racism, Xenophobia, Homophobia, and Other Forms of Discrimination
Discrimination encompasses a spectrum of injustices directed at individuals because of their supposed attributes and can be thought of as a chronic stressor that impacts health. The Canadian Human Rights Commission defines discrimination as “actions or decisions that unfairly target individuals or groups based on factors like race, age, sexual orientation, gender identity, or disability” Footnote 153 . Within Canada, 35.7% of the population reported experiencing some form of discrimination or unfair treatment in 2022 Footnote 154 . For some individuals, multiple forms of discrimination may be experienced, at once, thus making difficult to identify the main reason for this unequal treatment Footnote 155 . This entangled form of “intersectional discrimination” relates to many systems of inequality and is sometimes linked to increased risk of mental health difficulties Footnote 155 Footnote 156 . Here we focus on racism, xenophobia, discrimination based on religious minority status (e.g., antisemitism or Islamophobia) and discrimination due to sexual orientation, all of which profoundly affect mental health Footnote 157 .
Racism and Xenophobia
Historical policies, stemming from unjust ideologies of racial hierarchies, led to discriminatory and often violent treatment of people, including Indigenous and racialized people Footnote 158 . The effects of these practices continue to drive, covertly and overtly, stigma, racism, and discrimination, especially against those with a racialized background Footnote 158 .
Racism is a powerful determinant of health and has been linked to inequalities affecting the mental health of racialized populations in a variety of ways. How people are valued , considered different or lesser, or treated unfairly is influenced by many layers of systems and structures that perpetuate racism at various societal levels (i.e., interpersonal, community, institutional, structural). Negative attitudes towards (prejudice), negative beliefs about (stereotypes), and differential treatment of (discrimination) nondominant racial groups by individuals and social institutions, especially those from or influenced by the dominant racial group, create the foundational elements for racism. In turn, racism can breed or exacerbate prejudice, negative stereotypes, and discrimination, further perpetuating harm against the nondominant racial group Footnote 159 Footnote 160 Footnote 161 .
According to Phelan & Link, racism is associated with health “largely via inequalities in power, prestige, freedom, neighborhood context, and health care” Footnote 165 .
Racism can be internalized (shame, sense of personal embarrassment, low self-esteem, or rejection of one’s identity or culture) , interpersonal (harassment, discrimination, or microaggressions between individuals), institutional and systemic (negative portrayals in media, overpolicing of specific communities, lack of diversity in positions of power, biases that shape socioeconomic status, and unequal access to opportunities) and structural. Structural racism includes factors such as interconnected systems of education, housing, employment, wealth, access to financial credit, immigration, and health care access; symbolic sources of advantage; and the distribution of resources Footnote 162 Footnote 163 Footnote 164 .
Racism is considered one of the fundamental root causes of differences in socio-economic status, resulting in mental, physical, and general health inequity Footnote 162 Footnote 165 . A 2015 meta-analysis, identified 5 pathways through which racism affects health: 1) reduced access to basic and social resources such as employment, housing, and education and/or increased exposure to risk factors; 2) worsening cognitive and/or emotional processes associated with mental illness; 3) increasing burden of chronic stress that, via pathophysiological processes, are related to disease; 4) reduced participation in health-promoting behaviours (e.g., sleep) and/or increased engagement in unhealthy behaviours (e.g., alcohol consumption) as a way of coping or self-regulation; and 5) increased physical harm as a result of racially motivated violence Footnote 162 . A contemporary and historical review of the implications of structural racism on health inequities provides a more expansive review of pathways, including economic injustice, environmental and occupational health inequities, political exclusion and targeted marketing of health-harming substances Footnote 163 .
Experiencing racism and discrimination has been consistently linked to depression, anxiety, chronic stress, psychological stress, negative affect, reoccurring negative emotions, and posttraumatic stress, among other outcomes Footnote 162 Footnote 163 . Black, Indigenous, and other racialized populations in North American, European, or other White-majority countries or Western societies can experience racial trauma, defined as the “repetitive, constant, inevitable, and cumulative” experiences across the life course of “threats, prejudices, harm, shame, humiliation and guilt,” leading to mental health outcomes of depression, anxiety, PTSD, and suicidal ideation, among others Footnote 164 . Everyday racial discrimination is associated with depressive symptoms among Black people in Canada Footnote 166 , and anti-Black racism in particular impacts the mental health of youth Footnote 167 .
Xenophobia is distinct from but related to racism. It has been defined as “attitudes, prejudices, and behaviour that reject, exclude, and often vilify persons, based on the perception that they are outsiders or foreigners to the community, society, or national identity” Footnote 168 Footnote 169 . Racism and xenophobia are phenomena that have shaped the systemic discrimination and socioeconomic marginalization of racialized Canadian-born and immigrant people Footnote 170 . Ideas about who belongs in a society are drivers of discrimination and anti-immigrant sentiments begin well before immigrants move to a new country. Newcomers to Canada face negative attitudes towards their countries of origin through the perpetuation of stereotypes linked to “Orientalism,“ or notions of Western superiority, and being a threat to Western cultures Footnote 134 .
Box 4.3: The enduring legacy of colonial structures and their impact on First Nations, Inuit, and Métis
Colonization has been widely recognized as a key determinant of health for Indigenous Peoples Footnote 171 Footnote 172 . The colonial structure, which has sought to assimilate Indigenous Peoples through the imposition of the dominant Euro-Canadian culture, laws, institutions, and systems, has been described as a mesh or a net of interconnected institutions that expands and contracts over time in its objective of establishing dominance. The institutions include government departments, churches, and corporations, and Indigenous communities encounter this mesh in many settings and via many ways. At times, the communities are caught in this net, and at other times they are able to slip between its strands Footnote 173 .
In this section, a distinctions-based approach has been applied to explore some of the ways in which First Nations, Inuit, and Métis have encountered this colonial mesh. While there are commonalities in terms of how colonialism has affected First Nations, Inuit, and Métis, including the loss of land, culture, and self-determination, encounters with colonial structures have not always been the same, as indicated by the analogy of the mesh that contracts in some places and expands in others. The events discussed are not meant to be a comprehensive historical retelling of the many complex ways in which the colonial structure affected and continues to affect Indigenous Peoples. Rather, they serve as examples of some of the unique ways in which Indigenous Peoples have been forced to face the challenges of colonialism.
First Nations
Land is central to the identity, spirituality, and well-being of First Nations in Canada. However, over the course of centuries, the British, French, and later the Canadian government, signed a series of treaties with First Nations that ultimately resulted in the systematic displacement and dispossession of Traditional and Ancestral Lands, leading to the forceful displacement of First Nations into remote communities and reserves that were often uninhabitable and lacking in resources Footnote 174 . The dispossession of First Nations’ land has had profound social, cultural, and economic consequences, disrupting traditional ways of life and contributing to the impoverishment of Indigenous communities Footnote 175 .
The Indian Act of 1876 was introduced with the aim of defining the legal status and rights of Indigenous Peoples. However, it did so in a way that curtailed the autonomy and cultural practices of First Nations. The Act established the Band Council system, wherein Indigenous communities were forced to adopt a Euro-Canadian model of governance. This system imposed elected leaders and council structures on First Nations communities, often in opposition to traditional governance systems Footnote 176 .
The Indian Act discriminated against First Nations women and sought to eliminate their autonomy in marriage and politics. The Act sought to reduce the number of Status Indians the Canadian government was responsible for by, among other ways, establishing that Indian status was transmitted through the patrilineal line. As a result, First Nations women could lose their status through marriage to non-First Nations spouses. They and their children were systemically denied access to their communities and the Treaty Rights they were entitled to. This resulted in the disempowerment of First Nations women, who previously wielded influence and played powerful roles within traditional structures Footnote 177 .
The Act also granted the Canadian government sweeping powers over Indigenous lands, resources, and finances. By establishing a system of reserves that confined Indigenous communities to designated areas and severely limited their control over their Traditional Territories, the Canadian government effectively stripped Indigenous communities of their ability to make decisions about land use, economic development, and resource management, further eroding self-determination. Treaties were often not honoured, and resources stemming from goods such as timber rights were not channelled back to the communities to invest in local services and infrastructure Footnote 176 .
The establishment of the Indian residential school system is one of the most egregious aspects of the Indian Act. Established in the late 19th century, these government-sponsored and church-run institutions forcibly separated Indigenous children from their families and communities, with the goal of erasing Indigenous cultures and languages. The physical, emotional, and psychological abuse suffered by First Nations children in these schools has had intergenerational effects, leading to trauma, substance abuse, and mental health challenges within Indigenous communities Footnote 172 . More than 150,000 Indigenous children attended residential schools between 1857 and 1996.
The Canadian government and Christian churches also established and enforced Indian day schools. These schools shared the same objectives as residential schools of erasing Indigenous cultures and languages, but as the name suggests, the children attended these schools normally returned home to their communities at the end of each school day Footnote 178 .
The Sixties Scoop, which occurred mostly in the 1960s and 1970s, represents a tragic extension of these colonial policies. Under the guise of child welfare, many First Nations children were forcibly removed from their families and communities, exacerbating the damage done by the Indian Act and the residential school system. These children were often placed in non-Indigenous foster homes or adopted by non-Indigenous families, resulting in a profound cultural disconnect and loss of identity. The enduring impact of the Sixties Scoop, characterized by intergenerational trauma and a struggle for cultural revitalization, underscores the continuation of colonial practices aimed at erasing Indigenous identities and autonomy Footnote 179 .
First Nations languages describe all aspects of creation such as the earth, stars, water, and fire as living, animate beings. As living beings, everything in this world has a unique identity, and within their identity is a description of their relationship to everything else, their purpose, and their meaning. In this manner, First Nations languages mediate and inform First Nations peoples’ ways of seeing, relating, and being in this world Footnote 11 . By attempting to erode First Nations languages and culture, colonial structures sought to erase the foundation of the identity of First Nations.
Inuit
Starting in the 1950s, Inuit in the Qikiqtani region were forced to relocate from their Traditional Territories to 13 permanent settlements created by the Canadian government in the High Arctic Footnote 180 . Inuit were not told how far they would be moving, how different their new homes would be, or that they would be separated from their extended families. They were not provided with adequate shelter and supplies. Moreover, the Canadian government reneged on its promise to return back to their old homes anyone who did not wish to stay. Because of the relocation, Inuit had to transition from a predominantly relations-based hunting culture based on reciprocity, where camps and sled dogs played a central role, to the commodity-based systems in towns and settlements.
Starting in the 1920s, Canadian authorities in the Arctic introduced a number of ordinances to regulate qimmiit (sled dogs) using as an excuse the need to protect people from dog attacks. In practice, this led to the killing of sled dogs, which were not only essential for hunting and relocating from one place to another, but which also played an important spiritual role for Inuit. By replacing dogs with snowmobiles, an alien economic system of commodities was imposed on Inuit, with concerns for snowmobile parts, fuel, and money replacing reciprocity and ningiqtuq (sharing) relations. The imposition of this system was part of a broader effort to assimilate Inuit to Western norms, values, assumptions, institutions, and ways of life. As a result, Inuit went from “a world impregnated with ritual, relationship, and meaning to one of impersonal, secular commodity relations” Footnote 181 . The detrimental impact of these policies was eventually recognized by the Government of Canada, which officially apologized in 2019 Footnote 182 .
From the 1940s to the 1960s, tuberculosis in Canada was at epidemic proportions. From the 1940s onwards, the Canadian government implemented a survey of Inuit and other Indigenous Peoples living in northern Canada to identify those who had tuberculosis and other serious conditions. People with these conditions were taken away from their homes and their families and were evacuated to hospitals in southern Canada. Hospital stays were often lengthy, often lasting several years, and while many Inuit returned home, others never did, either because they chose to stay in the south, because their health did not allow for them to return, or because they had died as a result of their illness. Inuit patients did not have the support of their families while undergoing treatment and had to adjust to a new culture as well as their illness and treatment at the hospital. Returning home entailed another series of readaptation challenges Footnote 183 .
Métis
Relationships with the land are a central component of identity and wellness for Métis peoples, but past and ongoing assimilative strategies have served to disconnect, relocate, and displace the Métis from the land Footnote 184 . Métis peoples were moved to create space for European settlers, and they were excluded from treaty processes, removing their ability to bargain and uphold their collective rights. Attempts by the Métis to push back on this encroachment through political mobilization were met with military force, leading to clashes in Mica Bay, Red River, and Batoche. A system of scrip was instituted to parcel off small sections of agriculturally unproductive land in Manitoba to Métis people, which led to the further alienation and displacement of Métis families and communities Footnote 56 .
The Métis were discriminated against by colonial settlers who refused to integrate them under the standard school system. Instead, Métis children were forcefully removed from their families to attend residential and church-run schools. The children who were forced to attend these schools were often selected based on their appearance, with those who looked more like their European ancestors being spared Footnote 186 . Residential schools were set up to “civilize and Christianise” children and systematically erode Métis languages, traditions, spirituality, and culture Footnote 185 . Many Métis children experienced emotional, spiritual, physical, and sexual abuse, and the result trauma continues to affect the health and wellness of survivors and their descendants Footnote 187 .
Islamophobia
An example of intersectional discrimination discussed in Canadian mental health literature pertains to experiences of Islamophobia in Canadian society, with implications for perceptions of stress, safety, community belonging and connectedness, and self-esteem Footnote 188 . We deliberately chose to elaborate on this complex issue to describe how the multidimensional nature of intersecting forms of discrimination are experienced.
Islamophobia has been defined as the “dread, hatred, and hostility towards Islam and Muslims perpetrated by a series of closed views that imply and attribute negative and derogatory stereotypes and beliefs to Muslims … which results in practices of exclusion and discrimination” Footnote 189 . Canada’s anti-racism strategy (2024 – 2028) states that Islamophobia “includes racism, stereotypes, prejudice, fear or acts of hostility directed towards individual Muslims or followers of Islam in general” Footnote 190 . In addition to individual acts of intolerance and racial profiling, Islamophobia can lead to viewing and treating Muslims as a greater security threat on an institutional, systemic, and societal level Footnote 190 . Discrimination can be direct, for example, with “members of Muslim communities … explicitly denied a right or a freedom,” including the right to personal safety, or indirect, where an “uneven effect is produced for Muslims by a measure in place, even though this was not the explicit intention of whoever enacted the measure” Footnote 189 . Anti-Muslim hate crimes, which have been on the rise in Canada, are a form of direct discrimination, as are microaggressions Footnote 191 Footnote 192 .
In Western societies such as Canada, Islamophobia positions Muslims as “other” through several mechanisms. First, anti-Muslim sentiment intersects with systemic racism. As many Muslims are racialized, they may be othered in contrast to a local-born White identity Footnote 193 Footnote 194 , and Muslim identity is perceived as threatening to “local” White identity Footnote 194 . Second, social and public discourse, including media content, can reinforce perceived incompatibilities between Islamic and Western “values and ways of life” Footnote 194 , including in secular states where some people may feel apprehensive about the potential incursion of religion into public institutions and the public sphere Footnote 189 . Third, in the context of histories of armed conflicts in Muslim-majority countries, immigrants coming from countries with which Canada and similar states are or have been at conflict with are portrayed as a potential threat to national security Footnote 194 . Although, clearly “not all Arabs are Muslim, nor all Muslims, Arab” Footnote 194 , the 9/11 attacks in the United States and subsequent invasions and wars in Arab- or Muslim-majority states such as Iraq and Afghanistan have led to a conflation of “race, religion, and nationality” felt by both Arabs and Muslims in the post-9/11 period. This translates into experiences of Islamophobic discrimination Footnote 194 .
Indeed, the distinction between discrimination against Muslims and against ethnic or racial identities can be difficult to disentangle Footnote 189 . Canadian studies have noted the intersectional nature of Islamophobia-informed discrimination—particularly how discrimination occurs based on gender and visible markers of faith, such as wearing of the hijab, and on markers of race/ethnicity such as skin colour or accent Footnote 188 . A participant in a study of discrimination and Muslim women’s mental health explained:
For the visible ones, hijabi dressed in non-Canadian outfits, visibly different complexion, and an accent is a killer.… Different colour too. It’s a killer. That’s the worst possible avenue. You can have different layers, so if somebody is wearing a hijab and they don't have an accent, they have a better chance of being accepted than somebody who has a hijab and an accent. So, it kind of tops it all up Footnote 188 .
Another participant observed:
I feel like skin colour always plays a big part too. Muslim, you have a hijab, you have colour in your skin … There’s the Muslim part, and then there is skin colour, right. Put those together, it’s like people don’t know how to act anymore, right. That plays a big part in discrimination towards the Muslim community for sure Footnote 188 .
Participants in Hunt et al.’s study described being on the receiving end of microaggressions, including being asked questions about their country of origin or hearing comments about their assumed belonging to the community Footnote 188 :
And, they're going to think of me as a foreigner. Like, “Did you just move here?” I’m like “No, I've been living here … I [was] born here.” … I get that so much, and it’s like, why? Is it because I wear a niqab? Footnote 188 .
Other times, interpersonal experiences of discrimination are more overt, and include experiences of verbal abuse:
I remember this one time. Very recent time, … somebody, like, literally started swearing at me. Like telling me to take off my scarf Footnote 188 .
These types of interactions impact mental health and well -being , including affective health (mood) and sense of community belonging and self-esteem Footnote 188 . In the same study, one Muslim woman observed:
It has a huge impact on mental health, I feel because, you know, there are days when you’re just feeling down in general, and then, to have that added weight of, you know, whatever it is … sometimes it gets to be too much. It’s overwhelming in a day, you know. So, I think it’s a big impact on mental health Footnote 188 .
Discrimination Experienced by Newcomers to Canada
In a study of the mental health of young immigrant and refugee men described the social context of mental health as being the combination of “social structures, institutional practices and personal biographies.” For newcomers to Canada, feeling like an outsider and being misunderstood were common Footnote 134 . Stereotypical notions of lower- and middle-income countries being unsafe, less developed, and lacking modernity paint them as “backward,” undesirable, and lesser, which can stoke xenophobia. Conversely, these stereotypes create ideas that contribute to the expectations that newcomers should be grateful to be in Canada, adhere to ideas of good citizenship, and conform to and fit into Canadian society. This adds more stress and pressure to the experience of migration and settlement, which is often challenging and stressful in itself Footnote 134 . A participant in one study examining mental health among immigrant and refugee men described his experience as follows:
I kept telling [my lawyer] that I want to bring my family… I know their life is in danger. He told me, all you have to do is focus on yourself. Just stay away from trouble, always try to get a good education, be a nice citizen…. If you follow all those rules, then you might possibly … there are more chances to bring your family…. You have to be good citizen, you have to have a good income, support them … because the government, they don’t want to take care of other people, you know? Footnote 134
The process of migration and settlement, when complicated by xenophobia and racism, can lead to internalizing negative stereotypes and beliefs, reinforcing expectations to aspire to “whiteness,” or the normalization that White people’s social and cultural practices are the “correct” way. When perceived as a measure of success in society, this can lead to chronic exposure to stress and feelings of inferiority Footnote 195 .
In addition to employment and income-related challenges, immigrants, particularly those without official documentation, can experience barriers to accessing health care, adequate housing, and language classes Footnote 196 Footnote 197 . These precarious social conditions can lead to social isolation and dependence on either spouses or family members Footnote 197 . For example, a study of immigrant and refugee women who sought help for postpartum depression documented how a fear of deportation or withdrawal of residency status prevented some women from accessing necessary mental health supports. One participant noted:
I don’t have insurance. It’s been 9 months since I have given birth.… I need a Pap smear but I just don’t have support. I don’t have papers so it causes a lot of difficulties when you can’t go to school and you can’t learn English…. Not working, I was very depressed because … like right now I don’t have electricity, it was disconnected, I don’t have the money to pay for it. I tried to ask for assistance at immigration services, but I don’t have papers Footnote 197 .
When mental health inequalities by race and/or ethnicity and immigration status rely on self-reported survey data, response and sampling biases potentially occur. These, in turn, can affect the size of observed inequalities and make findings less valid and meaningful. For example, cultural perspectives may affect different people’s assertions and/or willingness to express thoughts about their mental health. Voluntary recruitment in survey designs can also lead to selective non-response (i.e., when non-participation occurs in clusters of respondents instead of individually) resulting in a group largely missing from data collection efforts. Addressing these issues requires capturing information on mental health through cross-culturally valid tools and employing methods to maximize survey participation. Taking these limitations into consideration, effect size of the observed inequalities should be interpreted with caution.
While the qualitative research speaks to how racism, discrimination, and xenophobia impact the mental health of racialized and immigrant Canadians, examination of the role of structural factors like systemic racism and discrimination on population mental health using quantitative approaches was beyond the scope of this report. We were, however, able to use CCHS data to present trends in positive mental health outcomes for racialized and immigrant population who experienced discrimination on the basis of race, ethnicity, culture, religion, and language.
Trends show that from 2009 to before 2022, average life satisfaction was lower among racialized and/or immigrant groups than White non-immigrants, for both males and females (Figure 6.A). However, these inequalities decreased over time and were no longer evident after the period 2017 to 2022. The overall prevalence of high self-reported mental health declined for all groups between 2007 and 2022, with females showing a steeper decline than males. Among both males and females, White non-immigrants showed the greatest reduction in high self-rated mental health over time and racialized immigrants reported the smallest reduction (Figure 6.B). This translated into notable decreases in high self-rated mental health inequality between racialized immigrants and White non-immigrants, in both absolute and relative terms, for both sexes.
Before 2022, White individuals (Canadian-born and immigrant) reported overall higher mean life satisfaction than racialized individuals (Figure 7.A). However, by 2020 to 2022 these differences were mostly no longer evident. Race/ethnicity-related inequalities in high self-rated mental health also decreased for most groups over time, most notably for Black males and females and South Asian males, (Figure 7.B). Narrowing racial/ethnic inequalities in life satisfaction tended to reflect improved life satisfaction scores in racialized populations compared to little change in life satisfaction scores in the White population. By contrast, high self-rated mental health declined in all groups, with narrowing racial/ethnic inequalities reflecting steeper declines in the White population than in other groups.
While the inequalities have decreased, declining mental health of the reference group is undesirable (also referred to as “levelling down”) Footnote 198 . This is an important consideration when assessing changes in inequalities over time. If levelling up is to be achieved, reducing inequalities should reflect improvements in positive mental health of those who are worse off as opposed to the experience of mental health deterioration among those that are better off.
Figure 6.A. Trends in mean life satisfaction by sex/gender, race/ethnicity, and immigrant status, population aged 12 years and older, 2009–2022
| Year | Sex | Group | Difference in mean life satisfaction score (95% CI) | Absolute change (95% CI) | Relative change |
|---|---|---|---|---|---|
| 2009-22 | Males | Non-immigrant, White (reference) | 0 | - | - |
| 2009-10 | Males | Non-immigrant, Racialized | -0.21 (-0.38, -0.04) | -0.14 (-0.39, 0.10) | -69 |
| 2011-13 | Males | Non-immigrant, Racialized | -0.08 (-0.22, 0.05) | ||
| 2014-16 | Males | Non-immigrant, Racialized | -0.26 (-0.44, -0.08) | ||
| 2017-19 | Males | Non-immigrant, Racialized | 0.04 (-0.08, 0.17) | ||
| 2020-22 | Males | Non-immigrant, Racialized | -0.07 (-0.24, 0.11) | ||
| 2009-10 | Males | Immigrant, White | -0.11 (-0.20, -0.03) | -0.17 (-0.30, -0.04) | -155 |
| 2011-13 | Males | Immigrant, White | -0.05 (-0.13, 0.03) | ||
| 2014-16 | Males | Immigrant, White | -0.09 (-0.16, -0.02) | ||
| 2017-19 | Males | Immigrant, White | 0.00 (-0.08, 0.07) | ||
| 2020-22 | Males | Immigrant, White | 0.06 (-0.04, 0.16) | ||
| 2009-10 | Males | Immigrant, Racialized | -0.24 (-0.35, -0.14) | -0.32 (-0.45, -0.18) | -131 |
| 2011-13 | Males | Immigrant, Racialized | -0.42 (-0.50, -0.33) | ||
| 2014-16 | Males | Immigrant, Racialized | -0.27 (-0.36, -0.18) | ||
| 2017-19 | Males | Immigrant, Racialized | -0.11 (-0.17, -0.04) | ||
| 2020-22 | Males | Immigrant, Racialized | 0.08 (0.0, 0.16) | ||
| 2009-22 | Females | Non-immigrant, White (reference) | 0 | - | - |
| 2009-10 | Females | Non-immigrant, Racialized | -0.31 (-0.53, -0.10) | -0.15 (-0.42, 0.13) | -47 |
| 2011-13 | Females | Non-immigrant, Racialized | -0.16 (-0.33, 0.02) | ||
| 2014-16 | Females | Non-immigrant, Racialized | -0.03 (-0.18, 0.12) | ||
| 2017-19 | Females | Non-immigrant, Racialized | -0.03 (-0.16, 0.10) | ||
| 2020-22 | Females | Non-immigrant, Racialized | -0.17 (-0.33, 0) | ||
| 2009-10 | Females | Immigrant, White | -0.21 (-0.29, -0.13) | -0.18 (-0.31, -0.06) | -88 |
| 2011-13 | Females | Immigrant, White | -0.22 (-0.29, -0.15) | ||
| 2014-16 | Females | Immigrant, White | -0.13 (-0.21, -0.05) | ||
| 2017-19 | Females | Immigrant, White | -0.09 (-0.16, -0.01) | ||
| 2020-22 | Females | Immigrant, White | -0.03 (-0.11, 0.06) | ||
| 2009-10 | Females | Immigrant, Racialized | -0.32 (-0.41, -0.22) | -0.40 (-0.52, -0.28) | -127 |
| 2011-13 | Females | Immigrant, Racialized | -0.34 (-0.42, -0.26) | ||
| 2014-16 | Females | Immigrant, Racialized | -0.23 (-0.30, -0.16) | ||
| 2017-19 | Females | Immigrant, Racialized | -0.14 (-0.22, -0.06) | ||
| 2020-22 | Females | Immigrant, Racialized | 0.09 (0.01, 0.16) |
Abbreviations: CI, confidence interval; SD, score difference; CCHS, the Canadian Community Health Survey.
Notes:
Mean life satisfaction: reported level of satisfaction with life as a whole right now, on a scale of 0 to 10, where 0 means “very dissatisfied” and 10 means “very satisfied.” Negative values of the life satisfaction score differences (SDs) indicate absolute inequalities in life satisfaction over the full time series. A value of 0 indicates that no difference exists between groups on that mental health outcome at a given time point. Changes in inequality are expressed in both absolute and relative scales between only the first and last time periods.
Absolute change calculation: (SD in 2009–2010)−(SD in 2020–2022).
Relative (%) change calculation: 100×[(SD in 2009–2010)−(SD in 2020–2022)/(SD in 2009–2010)].
Absolute and relative change interpretation: positive values indicate an increasing trend in immigration and race/ethnicity-related inequalities in life satisfaction; negative values indicate a decreasing inequality trends.
Immigrant status was based on respondents reporting that they are landed immigrants/non-permanent residents or non-immigrants (Canadian born).
Racialized status was determined based on respondents reporting if they belonged to a specified racial/cultural group (i.e., Black, White, South Asian). Responses were subsequently grouped into racialized or White groups (Indigenous identity was excluded from these analyses).
Data are from annual waves of the Canadian Community Health Survey; population sample is aged 12+ years; estimates are age-standardized to the 2016 Census population using 5-year age intervals. Analyses excluded data from the 2007–2008 survey wave, which used a different life satisfaction scale. Caution is warranted when comparing estimates from cycles prior to 2015 and for data released 2022. We do not exclude the possibility that trends observed may have been influenced by different methodologies used in the CCHS, including a new sample design in 2015.
For more information on data and analysis considerations, refer to https://health-infobase.canada.ca/mental-health/inequalities/technical-notes.html . Inequality trends for other mental health outcomes (e.g., suicidality, depressive symptomatology, life stress) are shown in the accompanying online data tool at https://health-infobase.canada.ca/mental-health/inequalities/data-tool.html .
Figure 6.B. Trends in excellent/very good self-rated mental health by sex/gender, by race/ethnicity and immigrant status, population aged 12 years and older, 2007–2022
| Year | Sex | Group | Prevalence difference for excellent/very good self-rated mental health (95% CI) | Absolute change (95% CI) | Relative change |
|---|---|---|---|---|---|
| 2007-22 | Males | Non-immigrant, White (reference) | 0 | - | - |
| 2007-10 | Males | Non-immigrant, Racialized | -4.4 (-8.8, 0.1) | -1.4 (-8.9, 6.0) | -33 |
| 2011-13 | Males | Non-immigrant, Racialized | -3.0 (-8, 1.9) | ||
| 2014-16 | Males | Non-immigrant, Racialized | -3.9 (-8, 0.2) | ||
| 2017-19 | Males | Non-immigrant, Racialized | -0.5 (-4.5, 3.5) | ||
| 2020-22 | Males | Non-immigrant, Racialized | -2.9 (-8.9, 3.0) | ||
| 2007-10 | Males | Immigrant, White | 1.9 (0.4, 3.5) | -2.7 (-5.9, 0.6) | -139 |
| 2011-13 | Males | Immigrant, White | 2.9 (0.9, 5) | ||
| 2014-16 | Males | Immigrant, White | 0.9 (-1.4, 3.1) | ||
| 2017-19 | Males | Immigrant, White | 3.8 (1.7, 6) | ||
| 2020-22 | Males | Immigrant, White | 4.6 (1.8, 7.4) | ||
| 2007-10 | Males | Immigrant, Racialized | -2.8 (-4.9, -0.8) | -7.8 (-11.0, -4.7) | -278 |
| 2011-13 | Males | Immigrant, Racialized | -4.2 (-6.7, -1.7) | ||
| 2014-16 | Males | Immigrant, Racialized | -2.5 (-4.7, -0.3) | ||
| 2017-19 | Males | Immigrant, Racialized | 0.2 (-1.8, 2.1) | ||
| 2020-22 | Males | Immigrant, Racialized | 5.0 (2.6, 7.4) | ||
| 2007-22 | Females | Non-immigrant, White (reference) | 0 | - | - |
| 2007-10 | Females | Non-immigrant, Racialized | -3.7 (-7.5, 0.1) | 1.3 (-5.4, 7.9) | 34 |
| 2011-13 | Females | Non-immigrant, Racialized | -2.0 (-6.9, 2.9) | ||
| 2014-16 | Females | Non-immigrant, Racialized | 4.1 (0.2, 7.9) | ||
| 2017-19 | Females | Non-immigrant, Racialized | -1.7 (-5.7, 2.4) | ||
| 2020-22 | Females | Non-immigrant, Racialized | -5.0 (-10.4, 0.5) | ||
| 2007-10 | Females | Immigrant, White | -0.8 (-2.4, 0.7) | -3.5 (-6.9, -0.2) | -430 |
| 2011-13 | Females | Immigrant, White | -0.7 (-2.8, 1.4) | ||
| 2014-16 | Females | Immigrant, White | 1.0 (-1.1, 3.1) | ||
| 2017-19 | Females | Immigrant, White | 2.8 (0.6, 5.1) | ||
| 2020-22 | Females | Immigrant, White | 2.7 (-0.2, 5.7) | ||
| 2007-10 | Females | Immigrant, Racialized | -7.0 (-9.1, -4.8) | -11.6 (-15.0, -8.3) | -167 |
| 2011-13 | Females | Immigrant, Racialized | -5.6 (-7.7, -3.5) | ||
| 2014-16 | Females | Immigrant, Racialized | -4.7 (-6.9, -2.5) | ||
| 2017-19 | Females | Immigrant, Racialized | -0.2 (-2.4, 2.0) | ||
| 2020-22 | Females | Immigrant, Racialized | 4.7 (2.1, 7.3) |
Abbreviations: CI, confidence interval; PD, prevalence difference; SRMH, self-rated mental health; CCHS, Canadian Community Health Survey
Notes:
Excellent/very good self-rated mental health (SRMH): percent of the population who reported their mental health as “excellent” or “very good” (vs. “good” or “fair” or “poor”). Negative values of the prevalence differences (PDs) indicate absolute inequality in excellent/very good SRMH over the full time series. A value of 0 indicates that no difference exists between groups on that mental health outcome at a given time point. Changes in inequality are expressed in both absolute and relative scales between only the first and last time periods
Absolute change calculation: (PD in 2007–2010)−(PD in 2020–2022).
Relative (%) change calculation: 100×[(PD in 2007–2010)−(PD in 2020–2022)/(PD in 2007–2010)].
Absolute and relative change interpretation: positive values indicate an increasing trend in immigration and race/ethnicity-related inequalities in excellent/very good SRMH, and negative values indicate a decreasing inequality trend.
Immigrant status was based on respondents reporting that they are landed immigrants/non-permanent residents or non-immigrants (Canadian born).
Racialized status was determined based on respondents reporting if they belonged to a specified racial/cultural group (i.e., Black, White, South Asian). Responses were subsequently grouped into racialized or White groups (Indigenous identity was excluded from these analyses).
Data are from annual waves of the Canadian Community Health Survey; population sample is aged 12+ years; estimates are age-standardized to the 2016 Census population using 5-year age intervals. Caution is warranted when comparing estimates from cycles prior to 2015 and for data released 2022. We do not exclude the possibility that trends observed may have been influenced by different methodologies used in the CCHS, including a new sample design in 2015.
For more information on data and analysis considerations, refer to https://health-infobase.canada.ca/mental-health/inequalities/technical-notes.html . Inequality trends for other mental health outcomes (e.g., suicidality, depressive symptomatology, life stress) are shown in the accompanying online data tool at https://health-infobase.canada.ca/mental-health/inequalities/data-tool.html .
Figure 7.A Trends in mean life satisfaction by sex/gender and race/ethnicity, population aged 12 years and older, 2009–2022
| Year | Sex | Group | Difference in mean life satisfaction score | Absolute change (95% CI) | Relative change |
|---|---|---|---|---|---|
| 2009-22 | Males | White (reference) | 0 | - | - |
| 2009-10 | Males | Black | -0.23 (-0.42, -0.03) | -0.15 (-0.40, 0.10) | -66 |
| 2011-13 | Males | Black | -0.06 (-0.25, 0.12) | ||
| 2014-16 | Males | Black | -0.08 (-0.25, 0.09) | ||
| 2017-19 | Males | Black | -0.17 (-0.34, -0.01) | ||
| 2020-22 | Males | Black | -0.08 (-0.24, 0.08) | ||
| 2009-10 | Males | Arab/West Asian | -0.22 (-0.51, 0.08) | 0.06 (-0.28, 0.40) | 26 |
| 2011-13 | Males | Arab/West Asian | -0.66 (-0.90, -0.42) | ||
| 2014-16 | Males | Arab/West Asian | -0.75 (-0.99, -0.51) | ||
| 2017-19 | Males | Arab/West Asian | -0.28 (-0.47, -0.08) | ||
| 2020-22 | Males | Arab/West Asian | -0.27 (-0.44, -0.10) | ||
| 2009-10 | Males | East/Southeast Asian | -0.39 (-0.53, -0.25) | -0.40 (-0.57, -0.23) | -103 |
| 2011-13 | Males | East/Southeast Asian | -0.43 (-0.55, -0.32) | ||
| 2014-16 | Males | East/Southeast Asian | -0.30 (-0.42, -0.19) | ||
| 2017-19 | Males | East/Southeast Asian | -0.25 (-0.35, -0.15) | ||
| 2020-22 | Males | East/Southeast Asian | 0.01 (-0.09, 0.11) | ||
| 2009-10 | Males | South Asian | -0.14 (-0.32, 0.04) | -0.33 (-0.56, -0.11) | -232 |
| 2011-13 | Males | South Asian | -0.36 (-0.51, -0.21) | ||
| 2014-16 | Males | South Asian | -0.18 (-0.35, -0.01) | ||
| 2017-19 | Males | South Asian | -0.03 (-0.15, 0.08) | ||
| 2020-22 | Males | South Asian | 0.19 (0.06, 0.32) | ||
| 2009-10 | Males | Latin American | -0.27 (-0.77, 0.23) | -0.66 (-1.25, -0.07) | -244 |
| 2011-13 | Males | Latin American | -0.28 (-0.85, 0.28) | ||
| 2014-16 | Males | Latin American | 0.22 (-0.08, 0.52) | ||
| 2017-19 | Males | Latin American | 0.08 (-0.15, 0.32) | ||
| 2020-22 | Males | Latin American | 0.39 (0.07, 0.71) | ||
| 2009-10 | Males | Other race/ethnicity or mixed origin | -0.12 (-0.33, 0.10) | 0.15 (-0.18, 0.47) | 128 |
| 2011-13 | Males | Other race/ethnicity or mixed origin | -0.11 (-0.31, 0.09) | ||
| 2014-16 | Males | Other race/ethnicity or mixed origin | -0.28 (-0.44, -0.12) | ||
| 2017-19 | Males | Other race/ethnicity or mixed origin | -0.10 (-0.23, 0.03) | ||
| 2020-22 | Males | Other race/ethnicity or mixed origin | -0.26 (-0.50, -0.02) | ||
| 2009-22 | Females | White (reference) | 0 | - | - |
| 2009-10 | Females | Black | -0.40 (-0.60, -0.20) | -0.54 (-0.79, -0.28) | -134 |
| 2011-13 | Females | Black | -0.27 (-0.47, -0.07) | ||
| 2014-16 | Females | Black | -0.14 (-0.33, 0.05) | ||
| 2017-19 | Females | Black | -0.19 (-0.34, -0.04) | ||
| 2020-22 | Females | Black | 0.14 (-0.01, 0.28) | ||
| 2009-10 | Females | Arab/West Asian | -0.47 (-0.89, -0.06) | -0.37 (-0.87, 0.13) | -78 |
| 2011-13 | Females | Arab/West Asian | -0.41 (-0.66, -0.17) | ||
| 2014-16 | Females | Arab/West Asian | -0.64 (-0.96, -0.32) | ||
| 2017-19 | Females | Arab/West Asian | -0.27 (-0.49, -0.05) | ||
| 2020-22 | Females | Arab/West Asian | -0.10 (-0.39, 0.18) | ||
| 2009-10 | Females | East/Southeast Asian | -0.30 (-0.41, -0.19) | -0.33 (-0.47, -0.19) | -108 |
| 2011-13 | Females | East/Southeast Asian | -0.34 (-0.44, -0.24) | ||
| 2014-16 | Females | East/Southeast Asian | -0.23 (-0.32, -0.13) | ||
| 2017-19 | Females | East/Southeast Asian | -0.08 (-0.17, 0.01) | ||
| 2020-22 | Females | East/Southeast Asian | 0.03 (-0.06, 0.11) | ||
| 2009-10 | Females | South Asian | -0.34 (-0.54, -0.14) | -0.43 (-0.68, -0.18) | -126 |
| 2011-13 | Females | South Asian | -0.20 (-0.35, -0.06) | ||
| 2014-16 | Females | South Asian | -0.21 (-0.37, -0.05) | ||
| 2017-19 | Females | South Asian | -0.14 (-0.28, -0.01) | ||
| 2020-22 | Females | South Asian | 0.09 (-0.06, 0.23) | ||
| 2009-10 | Females | Latin American | -0.22 (-0.75, 0.30) | -0.66 (-1.24, -0.08) | -294 |
| 2011-13 | Females | Latin American | -0.13 (-0.36, 0.09) | ||
| 2014-16 | Females | Latin American | -0.09 (-0.28, 0.11) | ||
| 2017-19 | Females | Latin American | 0.12 (-0.09, 0.32) | ||
| 2020-22 | Females | Latin American | 0.43 (0.19, 0.68) | ||
| 2009-10 | Females | Other race/ethnicity or mixed origin | -0.25 (-0.48, -0.03) | 0.05 (-0.25, 0.36) | 29 |
| 2011-13 | Females | Other race/ethnicity or mixed origin | -0.30 (-0.46, -0.14) | ||
| 2014-16 | Females | Other race/ethnicity or mixed origin | -0.13 (-0.26, 0) | ||
| 2017-19 | Females | Other race/ethnicity or mixed origin | -0.29 (-0.43, -0.14) | ||
| 2020-22 | Females | Other race/ethnicity or mixed origin | -0.30 (-0.51, -0.10) |
Abbreviations: CI, confidence interval; SD, score difference; CCHS, Canadian Community Health Survey.
Notes:
Mean life satisfaction: reported level of satisfaction with life as a whole right now, on a scale of 0 to 10, where 0 means “very dissatisfied” and 10 means “very satisfied.” Negative values of the life satisfaction score differences (SDs) indicate absolute inequalities in life satisfaction over the full time series. A value of 0 indicates that no difference exists between groups on that mental health outcome at a given time point. Changes in inequality are expressed in both absolute and relative scales between only the first and last time periods.
Absolute change calculation: (SD in 2009–2010)−(SD in 2020–2022).
Relative (%) change calculation: 100×[(SD in 2009–2010)−(SD in 2020–2022)/(SD in 2009–2010)].
Absolute and relative change interpretation: positive values indicate an increasing trend in immigration and race/ethnicity-related inequalities in life satisfaction; negative values indicate a decreasing inequality trends.
Race/ethnicity was determined based on responses to a question asking respondents with which group(s) they identify: South Asian, Chinese, Black, Filipino, Latin American, Arab, White, Southeast Asian, West Asian, Korean, Japanese, and other (specify). In our categorization, only respondents who self-identified as belonging to only 1 population group were categorized in that group (i.e., anyone identifying as belonging to 2 or more groups were categorized as “mixed origin”).
Data are from annual waves of the Canadian Community Health Survey; population sample aged 12+ years; estimates are age-standardized to the 2016 Census population using 5-year age intervals. Analyses excluded data from the 2007–2008 survey wave, which used a different life satisfaction scale. Caution is warranted when comparing estimates from cycles prior to 2015 and for data released 2022. We do not exclude the possibility that trends observed may have been influenced by different methodologies used in the CCHS, including a new sample design in 2015.
For more information on data and analysis considerations refer to https://health-infobase.canada.ca/mental-health/inequalities/technical-notes.html . Inequality trends for other mental health outcomes (e.g., suicidality, depressive symptomatology, life stress) by sex/gender and race/ethnicity are shown on the accompanying online data tool at https://health-infobase.canada.ca/mental-health/inequalities/data-tool.html .
Figure 7.B Trends in excellent/very good self-rated mental health by sex/gender and race/ethnicity, population aged 12 years and older, 2007–2022
| Year | Sex | Group | Prevalence difference for excellent/very good self-rated mental health (95% CI) | Absolute change (95% CI) | Relative change |
|---|---|---|---|---|---|
| 2007-22 | Males | White (reference) | 0 | - | - |
| 2007-10 | Males | Black | 0.3 (-4.3, 4.9) | -7.7 (-14.5, -0.8) | -2537 |
| 2011-13 | Males | Black | 2.0 (-2.5, 6.5) | ||
| 2014-16 | Males | Black | 5.4 (1, 9.7) | ||
| 2017-19 | Males | Black | 2.8 (-1.8, 7.4) | ||
| 2020-22 | Males | Black | 8.0 (2.9, 13) | ||
| 2007-10 | Males | Arab/West Asian | -3.6 (-9.1, 1.9) | -4.2 (-12.1, 3.6) | -117 |
| 2011-13 | Males | Arab/West Asian | -5.7 (-12.5, 1.1) | ||
| 2014-16 | Males | Arab/West Asian | -5.8 (-11.1, -0.5) | ||
| 2017-19 | Males | Arab/West Asian | -2.4 (-8.4, 3.6) | ||
| 2020-22 | Males | Arab/West Asian | 0.6 (-5.0, 6.2) | ||
| 2007-10 | Males | East/Southeast Asian | -4.1 (-6.6, -1.7) | -6.3 (-10.1, -2.4) | -151 |
| 2011-13 | Males | East/Southeast Asian | -8.0 (-11.5, -4.5) | ||
| 2014-16 | Males | East/Southeast Asian | -5.7 (-8.8, -2.7) | ||
| 2017-19 | Males | East/Southeast Asian | -5.2 (-8, -2.3) | ||
| 2020-22 | Males | East/Southeast Asian | 2.1 (-0.8, 5.1) | ||
| 2007-10 | Males | South Asian | -2.0 (-5.5, 1.4) | -9.1 (-14.1, -4.2) | -447 |
| 2011-13 | Males | South Asian | 0.1 (-3.9, 4.2) | ||
| 2014-16 | Males | South Asian | 1.1 (-2.8, 4.9) | ||
| 2017-19 | Males | South Asian | 4.0 (0.8, 7.3) | ||
| 2020-22 | Males | South Asian | 7.1 (3.6, 10.6) | ||
| 2007-10 | Males | Latin American | -5.5 (-12.1, 1.1) | -11.0 (-20.9, -1.1) | -201 |
| 2011-13 | Males | Latin American | -3.8 (-12.4, 4.8) | ||
| 2014-16 | Males | Latin American | 6.4 (-0.4, 13.2) | ||
| 2017-19 | Males | Latin American | 2.6 (-3.4, 8.7) | ||
| 2020-22 | Males | Latin American | 5.5 (-1.9, 12.9) | ||
| 2007-10 | Males | Other race/ethnicity or mixed origin | -2.9 (-7.7, 1.9) | 2.2 (-5.3, 9.7) | 64 |
| 2011-13 | Males | Other race/ethnicity or mixed origin | 0.9 (-3.6, 5.4) | ||
| 2014-16 | Males | Other race/ethnicity or mixed origin | -4.8 (-8.9, -0.7) | ||
| 2017-19 | Males | Other race/ethnicity or mixed origin | -1.2 (-5.1, 2.6) | ||
| 2020-22 | Males | Other race/ethnicity or mixed origin | 0.1 (-6.6, 6.7) | ||
| 2007-22 | Females | White (reference) | 0 | - | - |
| 2007-10 | Females | Black | -2.8 (-6.8, 1.1) | -10.2 (-16.4, -4.1) | -360 |
| 2011-13 | Females | Black | 3.3 (-1.3, 7.8) | ||
| 2014-16 | Females | Black | 0.9 (-3.8, 5.5) | ||
| 2017-19 | Females | Black | -0.1 (-4, 3.7) | ||
| 2020-22 | Females | Black | 7.4 (2.7, 12.1) | ||
| 2007-10 | Females | Arab/West Asian | -2.9 (-8.7, 2.8) | -5.4 (-13.8, 3.0) | -184 |
| 2011-13 | Females | Arab/West Asian | -7.2 (-13.4, -0.9) | ||
| 2014-16 | Females | Arab/West Asian | -7.3 (-14.4, -0.3) | ||
| 2017-19 | Females | Arab/West Asian | -2.4 (-8.7, 3.9) | ||
| 2020-22 | Females | Arab/West Asian | 2.5 (-3.7, 8.6) | ||
| 2007-10 | Females | East/Southeast Asian | -8.3 (-10.8, -5.7) | -13.4 (-17.4, -9.5) | -163 |
| 2011-13 | Females | East/Southeast Asian | -6.0 (-8.9, -3.2) | ||
| 2014-16 | Females | East/Southeast Asian | -4.8 (-7.7, -2.0) | ||
| 2017-19 | Females | East/Southeast Asian | -0.2 (-2.7, 2.4) | ||
| 2020-22 | Females | East/Southeast Asian | 5.2 (2.1, 8.2) | ||
| 2007-10 | Females | South Asian | -6.1 (-9.9, -2.2) | -10 (-15.9, -4.1) | -165 |
| 2011-13 | Females | South Asian | -5.2 (-9.2, -1.2) | ||
| 2014-16 | Females | South Asian | -2.4 (-6.3, 1.4) | ||
| 2017-19 | Females | South Asian | -0.8 (-4.6, 2.9) | ||
| 2020-22 | Females | South Asian | 3.9 (-0.5, 8.4) | ||
| 2007-10 | Females | Latin American | -4.6 (-11.8, 2.6) | -7.0 (-16.8, 2.9) | -152 |
| 2011-13 | Females | Latin American | -2.7 (-9, 3.7) | ||
| 2014-16 | Females | Latin American | -6.9 (-13.2, -0.6) | ||
| 2017-19 | Females | Latin American | -4.1 (-10.1, 2.0) | ||
| 2020-22 | Females | Latin American | 2.4 (-4.4, 9.1) | ||
| 2007-10 | Females | Other race/ethnicity or mixed origin | -3.4 (-7.6, 0.9) | 2.2 (-5.3, 9.7) | 64 |
| 2011-13 | Females | Other race/ethnicity or mixed origin | -4.7 (-9.6, 0.3) | ||
| 2014-16 | Females | Other race/ethnicity or mixed origin | 0.8 (-2.9, 4.5) | ||
| 2017-19 | Females | Other race/ethnicity or mixed origin | -4.3 (-8.1, -0.5) | ||
| 2020-22 | Females | Other race/ethnicity or mixed origin | -5.5 (-11.7, 0.6) |
Abbreviations: CI, confidence interval; PD, prevalence difference; SRMH, self-rated mental health; CCHS, Canadian Community Health Survey.
Notes:
Excellent/very good self-rated mental health (SRMH): percent of the population who reported their mental health as “excellent” or “very good” (vs. “good” or “fair” or “poor”). Negative values of the prevalence differences (PDs) indicate absolute race/ethnicity-related inequality in excellent/very good SRMH over the full time series. A value of 0 indicates that no difference exists between groups on that mental health outcome at a given time point. Changes in inequality are expressed in both absolute and relative scales between only the first and last time periods.
Absolute change calculation: (PD in 2007–2010)−(PD in 2020–2022).
Relative (%) change calculation: 100×[(PD in 2007–2010)−(PD in 2020–2022)/(PD in 2007–2010)].
Absolute and relative (%) change interpretation: positive values indicate an increasing trend in race/ethnicity-related inequalities in excellent/very good SRMH, while negative values indicate a decreasing inequality trend.
Race/ethnicity was determined based on responses to a question asking respondents with which group(s) they identify: South Asian, Chinese, Black, Filipino, Latin American, Arab, White, Southeast Asian, West Asian, Korean, Japanese, and other (specify). In our categorization, only respondents who self-identified as belonging to only 1 population group were categorized in that group (i.e., anyone identifying as belonging to 2 or more groups were categorized as “mixed origin”).
Data are from annual waves of the Canadian Community Health Survey; population sample aged 12+ years; estimates are age-standardized to the 2016 Census population using 5-year age intervals. Caution is warranted when comparing estimates from cycles prior to 2015 and for data released 2022. We do not exclude the possibility that trends observed may have been influenced by different methodologies used in the CCHS, including a new sample design in 2015.
For more information on data and analysis considerations refer to https://health-infobase.canada.ca/mental-health/inequalities/technical-notes.html . Inequality trends for other mental health outcomes (e.g., suicidality, depressive symptomatology, life stress) by race/ethnicity and sex/gender are shown in the accompanying online data tool at https://health-infobase.canada.ca/mental-health/inequalities/data-tool.html .
Discrimination Based on Sexual Orientation
Homophobia, transphobia, and heteronormativity act as drivers of stigma and discrimination that can result in poor mental health outcomes. Homophobia is the pathological fear of or aversion to people who experience same-sex attraction. Homophobia can result in hostile and harmful behaviour such as acts of social exclusion, physical violence, and derogatory verbal attacks Footnote 199 Footnote 200 . Heteronormativity at a structural level represents a long-standing ideological system that discriminates against, marginalizes , invalidates, or penalizes any non-heterosexual form of behaviour, identity, relationship, or community Footnote 71 Footnote 72 . Heterosexuality is seen as the norm and “standard” of sexual orientation , despite that every human culture over every historical period has included same- and different-sex sexual orientations.
Several mechanisms have been proposed to explain the associations between sexual orientation and negative mental health outcomes. Studies have noted that lesbian, gay, bisexual, and transgender people are more likely to experience sexual or physical violence. Such stressors can result in physical and/or psychological trauma that can negatively affect mental health throughout the life course Footnote 201 . The overlapping and interconnected systems of sexism, heteronormativity, and other systems of power, such as racism and ableism, create conditions where 2SLGBTQI+ populations—particularly those who are racialized, have a positive HIV/AIDS status, or have been diagnosed with a mental health condition—experience disproportionate stigma, discrimination, violence, and social exclusion Footnote 67 Footnote 68 Footnote 69 Footnote 191 Footnote 201 Footnote 202 Footnote 203 Footnote 204 Footnote 205 . These factors represent both sources of stress and barriers to accessing health-promoting resources and social supports.
The Minority Stress Model has been used to explain negative mental health outcomes, primarily for 2SLGBTQI+ people, linked to stigma, prejudice, and discrimination Footnote 206 . This model posits that lifetime stressors produced by a culture of heteronormativity and homophobia, such as chronic exposure to experiences of discrimination or violence, when combined with identity factors such as sexual orientation, can lead to negative mental health outcomes for 2SLGBTQI+ individuals, especially in the absence of support systems. Other examples of identity-related lifetime stressors include exposure to stigmatizing beliefs about sexual and gender minorities; internalized homophobia (e.g., feelings of shame about one’s sexual orientation); and concealment of identity. Experiences of discrimination are complex and can include early childhood trauma, for example, due to gender identity/expression change efforts, including so-called conversion therapy, and homophobic and transphobic bullying and childhood maltreatment in multiple settings Footnote 207 . Results of the 2018 Survey of Safety in Public and Private Spaces indicate that about 4 1% of gay, lesbian, and bisexual people living in Canada experienced childhood victimization compared with 27% of heterosexual respondents Footnote 208 . The fear of disclosing sexual orientation or gender identity to family members, peers, in educational settings, or when accessing health care, can be especially detrimental.
Our qualitative review included several studies that discussed the mental health effects on 2SLGBTQI+ individuals experiencing discrimination due to homophobia, transphobia, and heteronormativity. For those living in smaller towns or rural locations, these effects may be more pronounced because of a lack of appropriate health care services and providers or due to the practice of concealing sexual identity through “protective coping” because of confidentiality concerns, leading to increased likelihood of depressive disorders and suicidal ideation Footnote 209 Footnote 210 .
In a qualitative study exploring childhood trauma and suicidality among 2SLGBTQI+ women, Creighton et al. examined the complexity of multiple social locations and mental health inequities in Canada Footnote 211 . One study participant described how disclosing their sexual orientation and having to face the consequences of their foster family’s overt homophobia exacerbated her depression:
She’s [the foster mother] the main reason why I’ve been depressed my whole life, I think, because I knew I was abandoned by my family, and I knew at a young age that these people weren’t my family. I’m not sure if you wanted to tie this into being gay or whatever, but in the foster homes that I lived in, like, in this house, they always told me being gay is wrong, and just a lot of mental abuse. So, it just took me a long time to really come out. Footnote 211
Heteronormative standards of appearance and behaviour were another source of difficulty for participants in many studies. For instance, one qualitative study participant reflected on being subjected to heteronormative standards of appearance, with families shunning alternative expressions of gender identity:
The closet is suffocating me, but I’m still unsure if I will survive coming out. You know, it’s not just, “your hair is disgusting,” or “the way you’re dressing is disgusting.” So, I really internalized a lot of self-hatred at that time, and that was my second suicide attempt—because it’s the pain of just not being able to be who you are, and being so closely monitored. Footnote 211
Participants in a study of transgender individuals in addiction treatment settings also described encountering expectations of gender identity, presentation, and behaviours, resulting in feelings of social rejection, judgment, harassment, and a lack of belonging Footnote 212 . As one participant explained:
My counsellor said that I wasn’t being true to myself because I was not acting like a normal Two-Spirited person would, and I would argue with her, like, well not argue, but debate with her, how am I supposed to act? Am I supposed to stay here and pop a hip every time? [Interviewer: She was saying you weren’t feminine enough?]. Yeah, it was weird. I just didn’t really like talking about it and … she was rude. She was really, really rude. So yeah, I left. Footnote 212
Disclosing their sexual orientation resulted in anxiety and fear for many participants in numerous studies. Coming out and the possible repercussions and potential for changed relationships with family members and friends added to feelings of anxiety and ostracism.
I felt sick and insecure, and I felt so scared, terribly scared. And the insecurity is just, it’s beyond description, it’s just this vacant, void feeling in the pit of your stomach that is just so hollow... it is exhausting... it wears you down. It kills your spirit. It forced me to go [to see a psychologist]…. It was helpful to admit that I was gay, and I had never admitted it aloud up until that point... it took like 5 sessions to say it. Once it was said there was a portion of weight that was lifted off my shoulders, and yet the journey continues but that was the first step. Footnote 213
Intersecting social locations and identities contribute to mistreatment . A racialized 2SLGBTQI+ individual reported how their experiences of discrimination were compounded:
There was no [other] person of colour who identified as gay. I was the only out person on campus, so I was very visible, so I was like the gay Black kid on campus … and I think I struggled a lot, particularly because my only access to my gay identity was those with who I had contact with on campus, online, and magazines, and all of those forms of connection were dominated by White identities. So for me it felt very isolating Footnote 209 .
The experience of overlapping marginalizations, whether living in smaller communities or urban settings, is especially difficult to navigate. As one participant described:
The double whammy—and well of course in Halifax [Nova Scotia] I wasn't out—but the double whammy of being both Aboriginal and Black meant that no matter how clever I was, no matter how good my portfolio was—how well I presented myself—I was never going to get a break. I had walked to the crest of the MacDonald Bridge (or was it the MacKay?) and I stood there—it was rush hour—and I stood there until it got dark, waiting to throw myself over. And I knew if I stayed in Halifax, one day I would throw myself over. So I had to get out, I had to leave … If I had been out, I mean the triple whammy would have been devastating Footnote 214 .
Subgroups within 2SLGBTQI+ communities also face unique challenges. Bisexual and transgender individuals often encounter complex and distinct challenges, confronting biphobia and transphobia both within and outside of 2SLGBTQI+ communities Footnote 215 Footnote 216 Footnote 217 . Bisexual individuals can face skepticism and erasure, as their sexual orientation is frequently misunderstood or dismissed as a phase Footnote 216 Footnote 218 Footnote 219 . Within 2SLGBTQI+ communities, some individuals question the authenticity of bisexual identities, or label bisexual individuals as indecisive, or presume that they can easily access heterosexual privilege if they have an other-sex partner. This perceived lack of acceptance can be compounded when bisexual individuals are in heterosexual-presenting relationships and face a “double discrimination”—for their sexual orientation by heterosexuals, and for their relationship choices by homosexuals Footnote 218 .
Transgender individuals grapple with a unique form of discrimination as they face resistance from heteronormative society and from some members of 2SLGBTQI+ communities Footnote 215 Footnote 220 Footnote 221 . Transphobia can manifest as prejudice, misunderstanding, and even exclusion from spaces designated for queer individuals. This makes it difficult for transgender individuals to access crucial support networks, and also puts them at risk for increased violence and hate-fuelled crimes Footnote 215 Footnote 217 . In addition, many forms of discrimination that transgender people encounter are structural in nature or related to a built environment that favours gender conformity and heteronormativity Footnote 222 . This includes difficulties finding work because of discrimination, navigating bureaucratic systems and networks that rely on gender markers and identification, and using public restrooms, difficulties that greatly impact 2SLGBTQI+ youth, and particularly transgender and nonbinary people Footnote 222 .
The sexual orientation variable in the CCHS has evolved over the years, with expanded terminology and extended age eligibility for the sexual orientation question. For consistency across the different survey waves, we have maintained the age range (15–59 years) and categorization (“heterosexual,” “gay or lesbian,” and “bisexual”) from earlier waves. (For further details, refer to Technical Notes at https://health-infobase.canada.ca/mental-health/inequalities/technical-notes.html).
Analyses of CCHS data show that, individuals identifying as bisexual or gay/lesbian reported worse levels of positive mental health compared to those identifying as heterosexual. Those identifying as bisexual experienced the lowest levels of positive mental health of all groups. Trends or inequalities changes in high self-rated mental and life satisfaction by sexual orientation differed for males and females. The gap, or inequality, in high self-rated mental health between bisexual and heterosexual individuals increased between 2007-2010 and 2020-2022 for males and females (8.2 percentage points and 16.6 percentage points, respectively). On the other hand, there were no statistically significant inequalities between lesbian/gay and heterosexual individuals over the same time period for both males and females. This could be related to how rates fell among heterosexual individuals (closer to the levels of gay/lesbian individuals). Particularly, rates of high self-rated mental declined steadily over time, with rates falling from as high as 75.8% and 74.2% for males and females identifying as heterosexual, respectively, in 2007–2010 to 62.0% and 53.8%, respectively, by 2020-2022. This is an important point to understand when drawing conclusions from the results. Temporal dynamics of inequalities (i.e., widening, stability or narrowing of the divide in positive mental health) may be driven by worsening rates in the best-performing or reference group. This is often referred to as “levelling down” Footnote 198 which marks an undesirable change of inequalities (i.e., improvements should be seen by bringing up the level of positive mental health of those who are worse off to that of the best-performing group or “levelling up”).
Figure 8.A. Trends in mean life satisfaction score by sex/gender and sexual orientation, population aged 18–59 years, 2009–2022
| Year | Sex | Sexual Orientation | Difference in mean life satisfaction score | Absolute change (95% CI) | Relative change |
|---|---|---|---|---|---|
| 2009-22 | Males | Heterosexual (reference) | 0 | - | - |
| 2009-10 | Males | Gay/Lesbian | -0.17 (-0.37, 0.02) | 0.05 (-0.30, 0.34) | 27 |
| 2011-13 | Males | Gay/Lesbian | -0.17 (-0.36, 0.02) | ||
| 2014-16 | Males | Gay/Lesbian | -0.31 (-0.50, -0.12) | ||
| 2017-19 | Males | Gay/Lesbian | -0.15 (-0.33, 0.04) | ||
| 2020-22 | Males | Gay/Lesbian | -0.22 (-0.44, 0) | ||
| 2009-10 | Males | Bisexual | -0.36 (-0.64, -0.08) | 0.5 (0.11, 0.89) | 139 |
| 2011-13 | Males | Bisexual | -0.87 (-1.31, -0.44) | ||
| 2014-16 | Males | Bisexual | -0.43 (-0.66, -0.20) | ||
| 2017-19 | Males | Bisexual | -0.67 (-0.92, -0.42) | ||
| 2020-22 | Males | Bisexual | -0.86 (-1.13, -0.58) | ||
| 2009-22 | Females | Heterosexual (reference) | 0 | - | - |
| 2009-10 | Females | Gay/Lesbian | -0.10 (-0.31, 0.11) | 0.15 (-0.2, 0.48) | 151 |
| 2011-13 | Females | Gay/Lesbian | -0.24 (-0.43, -0.05) | ||
| 2014-16 | Females | Gay/Lesbian | -0.19 (-0.41, 0.03) | ||
| 2017-19 | Females | Gay/Lesbian | -0.34 (-0.54, -0.14) | ||
| 2020-22 | Females | Gay/Lesbian | -0.25 (-0.50, 0) | ||
| 2009-10 | Females | Bisexual | -0.77 (-1.14, -0.39) | 0.10 (-0.4, 0.56) | 149 |
| 2011-13 | Females | Bisexual | -0.76 (-1.10, -0.43) | ||
| 2014-16 | Females | Bisexual | -0.90 (-1.12, -0.68) | ||
| 2017-19 | Females | Bisexual | -0.83 (-1.12, -0.60) | ||
| 2020-22 | Females | Bisexual | -0.86 (-1.13, -0.59) |
Abbreviations: CI, confidence interval; SD, score difference; CCHS, Canadian Community Health Survey.
Notes:
Mean life satisfaction: reported level of satisfaction with life as a whole right now, on a scale of 0 to 10, where 0 means “very dissatisfied” and 10 means “very satisfied.” Negative values of the life satisfaction score differences (SDs) indicate absolute sexual minority vs. heterosexual inequalities in life satisfaction over the full time series. A value of 0 indicates that no difference exists between groups on that mental health outcome at a given time point. Changes in inequality are expressed in both absolute and relative scales between only the first and last time periods.
Absolute change calculation: (SD in 2009–2010)−(SD in 2020–2022).
Relative (%) change calculation: 100×[(SD in 2009–2010)−(SD in 2020–2022)/(SD in 2009–2010)].
Absolute and percent change interpretation: positive values indicate an increasing trend in sexual orientation inequalities in life satisfaction, negative values indicate a decreasing inequality trend.
Respondents reported on sexual orientation by choosing from the following predetermined categories: “heterosexual,” “gay or lesbian,” and “bisexual.” From 2019 to 2021, the Canadian Community Health Survey (CCHS) included pansexual individuals in the bisexual category but was removed in 2022.
Data are from annual waves of the CCHS; population sample is aged 18–59 years due to a restriction on respondents being asked the sexual orientation question prior to 2015; estimates are age-standardized to the 2016 Census population using 5-year age intervals. Analyses excluded data from the 2007–2008 survey wave, which used a different life satisfaction scale. Caution is warranted when comparing estimates from cycles prior to 2015 and for data released 2022. We do not exclude the possibility that trends observed may have been influenced by different methodologies used in the CCHS, including a new sample design in 2015.
For more information on data and analysis considerations refer to https://health-infobase.canada.ca/mental-health/inequalities/technical-notes.html . Inequality trends for other mental health outcomes (e.g., suicidality, depressive symptomatology, life stress) by sexual orientation are shown in the accompanying online data tool at https://health-infobase.canada.ca/mental-health/inequalities/data-tool.html .
Figure 8.B. Trends in excellent/very good self-rated mental health by sex/gender and sexual orientation, population aged 18–59 years, 2007–2022
| Year | Sex | Sexual Orientation | Prevalence difference for excellent/very good self-rated mental health | Absolute change (95% CI) | Relative change |
|---|---|---|---|---|---|
| 2007-22 | Male | Heterosexual (reference) | 0 | - | - |
| 2007-10 | Male | Gay/Lesbian | -2.9 (-7.4, 1.5) | 8.4 (0.9, 15.9) | 286 |
| 2011-13 | Male | Gay/Lesbian | -6.5 (-12.2, -0.9) | ||
| 2014-16 | Male | Gay/Lesbian | -5.4 (-11.0, 0.1) | ||
| 2017-19 | Male | Gay/Lesbian | -11.7 (-16.7, -6.6) | ||
| 2020-22 | Male | Gay/Lesbian | -11.4 (-17.4, -5.3) | ||
| 2007-10 | Male | Bisexual | -10.1 (-16.4, -3.9) | 8.2 (-1.3, 17.7) | 81 |
| 2011-13 | Male | Bisexual | -24.9 (-32.9, -16.9) | ||
| 2014-16 | Male | Bisexual | -16.7 (-23.8, -9.6) | ||
| 2017-19 | Male | Bisexual | -16.3 (-24.1, -8.5) | ||
| 2020-22 | Male | Bisexual | -18.3 (-25.5, -11.1) | ||
| 2007-22 | Female | Heterosexual (reference) | 0 | - | - |
| 2007-10 | Female | Gay/Lesbian | -2.5 (-7.3, 2.3) | 3.1 (-4.8, 10.9) | 123 |
| 2011-13 | Female | Gay/Lesbian | -3.7 (-10.0, 2.5) | ||
| 2014-16 | Female | Gay/Lesbian | -7.1 (-13.5, -0.8) | ||
| 2017-19 | Female | Gay/Lesbian | -6.6 (-11.8, -1.4) | ||
| 2020-22 | Female | Gay/Lesbian | -5.6 (-11.8, 0.7) | ||
| 2007-10 | Female | Bisexual | -15.8 (-21.1, -10.5) | 16.6 (9.3, 23.9) | 105 |
| 2011-13 | Female | Bisexual | -23.5 (-30.0, -17.1) | ||
| 2014-16 | Female | Bisexual | -23.7 (-29.2, -18.3) | ||
| 2017-19 | Female | Bisexual | -24.1 (-29.4, -18.8) | ||
| 2020-22 | Female | Bisexual | -32.4 (-37.4, -27.5) |
Abbreviations: CI, confidence interval; PD, prevalence difference; SRMH, self-rated mental health; CCHS, Canadian Community Health Survey.
Notes:
Excellent/very good self-rated mental health (SRMH): percent of the population who reported their mental health as “excellent” or “very good” (vs. “good” or “fair” or “poor”). Negative values of the prevalence differences (PDs) indicate absolute sexual minority vs. heterosexual inequality in excellent/very good SRMH over the full time series. A value of 0 indicates that no difference exists between groups on that mental health outcome at a given time point. Changes in inequality are expressed in both absolute and relative scales between only the first and last time periods.
Absolute change calculation: (PD in 2007–2010)−(PD in 2020–2022).
Relative (%) change calculation: 100×[(PD in 2007–2010)−(PD in 2020–2022)/(PD in 2007–2010)].
Absolute and relative change interpretation: positive values indicate an increasing trend in sexual orientation inequalities in excellent/very good SRMH, and negative values indicate decreasing inequality trends.
Respondents reported on sexual orientation by choosing from the following predetermined categories: “heterosexual,” “gay or lesbian,” and “bisexual.” From 2019 to 2021, the Canadian Community Health Survey (CCHS) included pansexual individuals in the bisexual category but was removed in 2022.
Data are from annual waves of the CCHS; population sample is aged 18–59 years due to a restriction on respondents being asked the sexual orientation question prior to 2015; estimates are age-standardized to the 2016 Census population using 5-year age intervals. Caution is warranted when comparing estimates from cycles prior to 2015 and for data released 2022. We do not exclude the possibility that trends observed may have been influenced by different methodologies used in the CCHS, including a new sample design in 2015.
For more information on data and analysis considerations refer to https://health-infobase.canada.ca/mental-health/inequalities/technical-notes.html . Inequality trends for other mental health outcomes (e.g., suicidality, depressive symptomatology, life stress) by sexual orientation are shown in the accompanying online data tool at https://health-infobase.canada.ca/mental-health/inequalities/data-tool.html .
4.1.3 Social and Cultural Connection, Support Networks, and Community Belonging
The World Health Organization has designated loneliness (a subjective dissatisfaction with one's social relationships Footnote 223 and social isolation (the objective lack of social contact, network size, and frequent social interaction Footnote 223 as a global public health concern, estimating that 1 in 4 older adults experience social isolation while 5 to 15 percent of adolescents experience loneliness Footnote 224 . The prevalence of Canadians aging without support is rising Footnote 225 and in the United States, isolation and loneliness have been deemed as urgent, public health concerns with large impacts on lower academic achievement for children and youth, poorer work performance for adults and increased health care spending across all population groups Footnote 226 . These reports have identified that increasing social connection between individuals and across groups/communities is necessary to address this burgeoning mental health issue Footnote 226 . As an important social determinant of health, social connection is inequitably distributed amongst populations, primarily due to structural and systemic inequities in schools, workplaces, neighbourhoods, public policies, and digital environments Footnote 226 . In this report, social connection is recognized as a social determinant of mental health and well-being, which we describe based on the Canadian qualitative research review and measure quantitatively through community belonging.
Our synthesis of the qualitative literature found that sense of community belonging—and other related factors such as social support from others, connection to one’s culture, and ideas of community more generally–had an important impact on self-reported mental health, life satisfaction, and combatting feelings of loneliness. Community belonging refers to an individual’s sense of acceptance, inclusion, and connection within their community or social environment Footnote 227 . Community belonging acts as a strong independent predictor of self-rated mental health Footnote 227 as it emphasizes the idea that individuals thrive when they feel a sense of attachment, support, and identification with the people and places around them. Conversely, community belonging can be considered an outcome of positive mental health. As captured in the studies reviewed, community belonging is conceptualized as a determinant of mental health. People who report a strong sense of belonging to their communities are typically more likely to report excellent or very good mental health Footnote 227 . In addition, our review revealed that feelings of community belonging are inequitably distributed across certain populations, such as racialized individuals, recent immigrants, and 2SLGBTQI+ individuals. For example, increasing community belonging directly contributed to reducing feelings of loneliness, improving mental health:
“The community room that is open every day, all day, that is so innovative and useful… There were days I was really depressed and really lonely and couldn’t do anything. And you’re in bed all day. And you get out, you come here.” Footnote 228
Our findings spanned a broad understanding of community belonging, and focused primarily on protective and strengthening factors, such as social support, feelings of connection and how they can be experienced to impact mental health.
The concept of community belonging acknowledges the significant impact that social connections and interactions have on mental well-being Footnote 229 . Indeed, the quality of social relationships that we foster can profoundly influence mental health outcomes. An individual’s environment and position within society affects their ability to form a strong sense of community belonging. It is crucial to acknowledge that social inequalities and power dynamics can significantly influence an individual’s sense of belonging. Social and economic disparities, racial discrimination, gender-based discrimination, and social exclusion can create barriers to community belonging for certain individuals or groups Footnote 229 Footnote 230 . Sociology and public health researchers emphasize the importance of addressing structural factors, such as access to and availability of community-driven spaces like community centres, parks, recreation centres to promote community belonging and mental well-being Footnote 231 .
In 2021 and 2022, almost one-half (47%) of Canadian Social Survey respondents reported a strong sense of community belonging, with significant variations over the life course and in different subpopulations Footnote 232 . For younger people aged 15 to 34 years, only between 37% and 44% reported having a strong sense of community belonging, while an even lower proportion of 2SLGBTQI+ individuals, 36%, reported their sense of community belonging as strong Footnote 232 . In comparison, other groups, such as newcomers, report higher rates of strong community belonging Footnote 232 . It is important to note that the challenges associated with isolation and lower sense of community belonging vary widely across the life course. In the public health context in Canada, fostering community belonging is an important strategy for promoting mental health and preventing mental illnesses across all ages and populations.
Respondents may interpret the CCHS question used to measure sense of community belonging in different ways because the term “local community” is not explicitly defined Footnote 222 . It is unclear how such differences in interpretation impact the associations between sense of community belonging and positive mental health outcomes Footnote 222 .
Analyses of CCHS data show a consistent association between reporting stronger sense of community belonging and better positive mental health outcomes (refer to Figures 9.A and 9.B). Clear gradients in life satisfaction and high self-rated mental health according to level of community belonging were evident over time, both for males and females. Over the years, the gap in both mean life satisfaction and high self-rated mental health widened among individuals with a somewhat strong, somewhat weak, and very weak sense of community belonging compared to those with a very strong sense of community belonging. Growing inequalities primarily reflect greater worsening of positive mental health over time among those reporting a very low sense of community belonging. However, it is important to reiterate the well-established bidirectional relationship between sense of community belonging and mental health, with each exerting a clear influence on the other.
Figure 9.A. Trends in mean life satisfaction by sex/gender and sense of community belonging, population aged 12 years and older, 2009–2022
| Year | Sex | Belonging | Difference in mean life satisfaction score | Absolute change (95% CI) | Relative change |
|---|---|---|---|---|---|
| 2009-22 | Male | Very strong belonging (reference) | 0 | - | - |
| 2009-10 | Male | Strong belonging | -0.36 (-0.42, -0.30) | 0.21 (0.13, 0.29) | 59 |
| 2011-13 | Male | Strong belonging | -0.30 (-0.36, -0.24) | ||
| 2014-16 | Male | Strong belonging | -0.40 (-0.45, -0.35) | ||
| 2017-19 | Male | Strong belonging | -0.43 (-0.48, -0.38) | ||
| 2020-22 | Male | Strong belonging | -0.57 (-0.63, -0.51) | ||
| 2009-10 | Male | Weak belonging | -0.73 (-0.80, -0.67) | 0.47 (0.37, 0.56) | 64 |
| 2011-13 | Male | Weak belonging | -0.75 (-0.81, -0.68) | ||
| 2014-16 | Male | Weak belonging | -0.89 (-0.96, -0.83) | ||
| 2017-19 | Male | Weak belonging | -0.91 (-0.97, -0.85) | ||
| 2020-22 | Male | Weak belonging | -1.20 (-1.27, -1.13) | ||
| 2009-10 | Male | Very weak belonging | -1.16 (-1.28, -1.05) | 0.96 (0.79, 1.13) | 82 |
| 2011-13 | Male | Very weak belonging | -1.22 (-1.32, -1.11) | ||
| 2014-16 | Male | Very weak belonging | -1.37 (-1.49, -1.26) | ||
| 2017-19 | Male | Very weak belonging | -1.48 (-1.60, -1.37) | ||
| 2020-22 | Male | Very weak belonging | -2.12 (-2.25, -2.00) | ||
| 2009-22 | Female | Very strong belonging (reference) | 0 | - | - |
| 2009-10 | Female | Strong belonging | -0.28 (-0.34, -0.22) | 0.25 (0.17, 0.34) | 90 |
| 2011-13 | Female | Strong belonging | -0.36 (-0.41, -0.31) | ||
| 2014-16 | Female | Strong belonging | -0.44 (-0.49, -0.39) | ||
| 2017-19 | Female | Strong belonging | -0.41 (-0.45, -0.36) | ||
| 2020-22 | Female | Strong belonging | -0.53 (-0.59, -0.47) | ||
| 2009-10 | Female | Weak belonging | -0.75 (-0.82, -0.68) | 0.48 (0.38, 0.57) | 63 |
| 2011-13 | Female | Weak belonging | -0.82 (-0.88, -0.76) | ||
| 2014-16 | Female | Weak belonging | -0.96 (-1.02, -0.91) | ||
| 2017-19 | Female | Weak belonging | -0.91 (-0.97, -0.86) | ||
| 2020-22 | Female | Weak belonging | -1.23 (-1.29, -1.16) | ||
| 2009-10 | Female | Very weak belonging | -1.10 (-1.20, -0.99) | 0.82 (0.65, 0.99) | 74 |
| 2011-13 | Female | Very weak belonging | -1.33 (-1.42, -1.23) | ||
| 2014-16 | Female | Very weak belonging | -1.49 (-1.60, -1.38) | ||
| 2017-19 | Female | Very weak belonging | -1.52 (-1.63, -1.40) | ||
| 2020-22 | Female | Very weak belonging | -1.91 (-2.04, -1.78) |
Abbreviations: CI, confidence interval; SD, score difference; CCHS, Canadian Community Health Survey.
Notes:
Mean life satisfaction: reported level of satisfaction with life as a whole right now, on a scale of 0 to 10, where 0 means “very dissatisfied” and 10 means “very satisfied.” Negative values of the life satisfaction score differences (SDs) indicate community belonging–related inequalities in life satisfaction over the full time series. A value of 0 indicates that no difference exists between groups on that mental health outcome at a given time point. Changes in inequality are expressed in both absolute and relative scales between only the first and last time periods.
Absolute change calculation: (score difference (SD) in 2009–2010)−(SD in 2020–2022).
Relative (%) change calculation: 100×[(SD in 2009–2010)−(SD in 2020–2022)/(SD in 2009–2010)].
Absolute and relative (%) change interpretation: positive values indicate an increasing trend in community belonging–related inequalities in life satisfaction; negative values indicate a decreasing trend in community belonging–related inequalities in life satisfaction.
Respondents reported their sense of belonging to their local community as “very strong,” “somewhat strong,” “somewhat weak,” or “very weak.”
Data are from the Canadian Community Health Survey ; population sample is aged 12+ years; estimates are age-standardized using 2016 Census 5-year age intervals. Analyses excluded data from the 2007–2008 survey wave, which used a different life satisfaction scale. Caution is warranted when comparing estimates from cycles prior to 2015 and for data released 2022. We do not exclude the possibility that trends observed may have been influenced by different methodologies used in the CCHS, including a new sample design in 2015.
For more information on data and analysis considerations refer to https://health-infobase.canada.ca/mental-health/inequalities/technical-notes.html . Inequality trends for other mental health outcomes (e.g., suicidality, depressive symptomatology, life stress) are shown in the accompanying online data tool at https://health-infobase.canada.ca/mental-health/inequalities/data-tool.html .
Figure 9.B. Trends in excellent/very good self-rated mental health by sex/gender and sense of community belonging, population aged 12 years and older, 2007–2022
| Year | Sex | Belonging | Prevalence difference | Absolute change (95% CI) | Relative change |
|---|---|---|---|---|---|
| 2007-22 | Males | Very strong belonging (reference) | 0 | - | - |
| 2007-10 | Males | Strong belonging | -5.2 (-6.2, -4.1) | 5.4 (3.3, 7.5) | 104 |
| 2011-13 | Males | Strong belonging | -5.3 (-6.8, -3.8) | ||
| 2014-16 | Males | Strong belonging | -6.5 (-7.9, -5.0) | ||
| 2017-19 | Males | Strong belonging | -6.6 (-8.0, -5.1) | ||
| 2020-22 | Males | Strong belonging | -10.6 (-12.4, -8.7) | ||
| 2007-10 | Males | Weak belonging | -12.2 (-13.4, -10.9) | 11.7 (9.3, 14.2) | 97 |
| 2011-13 | Males | Weak belonging | -12.1 (-13.8, -10.4) | ||
| 2014-16 | Males | Weak belonging | -15.2 (-17, -13.5) | ||
| 2017-19 | Males | Weak belonging | -16.2 (-18, -14.5) | ||
| 2020-22 | Males | Weak belonging | -23.9 (-26.0, -21.8) | ||
| 2007-10 | Males | Very weak belonging | -18.7 (-20.6, -16.8) | 16.6 (13.0, 20.1) | 89 |
| 2011-13 | Males | Very weak belonging | -21.6 (-24.1, -19.0) | ||
| 2014-16 | Males | Very weak belonging | -24.8 (-27.4, -22.2) | ||
| 2017-19 | Males | Very weak belonging | -26.4 (-28.9, -23.8) | ||
| 2020-22 | Males | Very weak belonging | -35.3 (-38.3, -32.3) | ||
| 2007-22 | Females | Very strong belonging (reference) | 0 | - | - |
| 2007-10 | Females | Strong belonging | -5.7 (-6.8, -4.7) | 6.8 (4.6, 9.0) | 119 |
| 2011-13 | Females | Strong belonging | -5.5 (-6.8, -4.1) | ||
| 2014-16 | Females | Strong belonging | -7.7 (-9.0, -6.3) | ||
| 2017-19 | Females | Strong belonging | -8.8 (-10.3, -7.4) | ||
| 2020-22 | Females | Strong belonging | -12.6 (-14.5, -10.6) | ||
| 2007-10 | Females | Weak belonging | -13.8 (-15.0, -12.5) | 12.5 (10.0, 14.9) | 91 |
| 2011-13 | Females | Weak belonging | -14.1 (-15.7, -12.4) | ||
| 2014-16 | Females | Weak belonging | -17.6 (-19.2, -16) | ||
| 2017-19 | Females | Weak belonging | -19.7 (-21.5, -18) | ||
| 2020-22 | Females | Weak belonging | -26.2 (-28.3, -24.1) | ||
| 2007-10 | Females | Very weak belonging | -19.0 (-20.8, -17.3) | 17.8 (14.5, 21.1) | 94 |
| 2011-13 | Females | Very weak belonging | -24.5 (-26.8, -22.3) | ||
| 2014-16 | Females | Very weak belonging | -27.3 (-29.8, -24.8) | ||
| 2017-19 | Females | Very weak belonging | -30.5 (-33.1, -27.9) | ||
| 2020-22 | Females | Very weak belonging | -36.9 (-39.7, -34.1) |
Abbreviations: CI, confidence interval; PD, prevalence difference; SRMH, self-rated mental health; CCHS, Canadian Community Health Survey.
Notes:
Excellent/very good self-rated mental health (SRMH): percent of the population who reported their mental health as “excellent” or “very good” (vs. “good” or “fair” or “poor”). Negative values of the prevalence differences (PDs) indicate absolute community belonging–related inequality in excellent/very good SRMH over the full time series. A value of 0 indicates that no difference exists between groups on that mental health outcome at a given time point. Changes in inequality are expressed in both absolute and relative scales between only the first and last time periods.
Absolute change calculation: (PD in 2007 –20 10)−(PD in 2020 –20 22).
Relative (%) change calculation: 100×[(PD in 2007
–20
10)−(PD in
2020
–20
22
1
)/(PD in 2007
–20
10)].
Absolute and relative (%) change interpretation: positive values indicate an increasing trend in community belonging–related inequalities in excellent/very good SRMH, while negative values indicate a decreasing inequality trend.
Respondents reported their sense of belonging to their local community as “very strong,” “somewhat strong,” “somewhat weak,” or “very weak.”
Data are from the Canadian Community Health Survey; population sample is aged 12+ years; estimates are age-standardized using 2016 Census 5-year age intervals. Caution is warranted when comparing estimates from cycles prior to 2015 and for data released 2022. We do not exclude the possibility that trends observed may have been influenced by different methodologies used in the CCHS, including a new sample design in 2015.
For more information on data and analysis considerations, refer to https://health-infobase.canada.ca/mental-health/inequalities/technical-notes.html . Inequality trends for other mental health outcomes (e.g., suicidality, depressive symptomatology, life stress) are shown in the accompanying online data tool at https://health-infobase.canada.ca/mental-health/inequalities/data-tool.html .
Cultural Connection and Social Supports for Immigrants
Immigrants may face multiple challenges related to building strong community ties upon arrival in their host country. These include their social identity (including connections, welcoming community, and ability to adapt to Canadian institutions), their personal history (such as their language and culture), and their socioeconomic context, among others Footnote 233 Footnote 234 . The process of integrating and feeling connected to the local community is crucial for overall well-being and successful adaptation to a new country. Our qualitative review highlighted barriers that may hinder community belonging, the role of social support networks, and the significance of support organizations in fostering inclusivity and challenging discriminatory practices.
Employment barriers due to systemic discrimination, including credential recognition and expectation of Canadian work experience, pose significant challenges in securing stable and meaningful jobs for many newcomers to Canada Footnote 234 Footnote 235 Footnote 236 . Any language barriers that make it difficult to effectively communicate, access essential services, and establish connections outside of people’s own ethnocultural communities can compound the problem Footnote 233 Footnote 234 . Moreover, experiences of discrimination, particularly among racialized immigrants, hinder social participation and exacerbate feelings of alienation Footnote 233 . In addition, economic shifts over the past decade have resulted in decreased worker protections, including decreased unionization, lack of benefits, and more short-term contractual work versus full-time employment. This has added impacts for recent immigrants and on the isolation of those living in Canada (see also Section 3.3.1.).
Recent immigrants typically find a sense of belonging within their ethnocultural communities in Canada before establishing connections in the broader geographic community or dominant society Footnote 233 . Ethnocultural or linguistic communities can provide initial support and familiarity and help newcomers navigate the complexities of their new surroundings Footnote 236 ; this means that residing in areas with a low density of ethnocultural community members who might provide initial support can make it more difficult to integrate into the wider community Footnote 233 Footnote 236 . Still, developing a sense of community belonging beyond a person’s ethnocultural community presents its own set of challenges: language barriers, employment difficulties, and experiences of discrimination make it arduous for immigrants to form new relationships with individuals who do not share similar cultural and linguistic roots Footnote 233 . Overcoming these challenges requires a comprehensive approach that addresses multiple aspects of immigrant life. As one immigrant service provider expressed:
I think for geographic community belonging, the newcomers or the new immigrants need time. That is the first step, it’s the ethnic community, and after that, geographic, and then after that, the third step, the Canadian society belonging. Footnote 233
The role of social support networks and social inclusion emerged as a protective factor for newcomers’ mental well-being. However, the immigrant services that foster these connections are often underfunded and understaffed and have limited mandates, resulting in gaps in their services Footnote 236 Footnote 237 .
A multitude of challenges impact community belonging for immigrants Footnote 223 Footnote 227 . Language barriers can hinder communication and integration into a community. Inability to find work or appropriate work puts financial strain on families and impedes integration. Overreliance on small ethnocultural communities may hinder integration if these groups lack social and economic capital.
Qualitative study findings consistently emphasized that individuals with a strong sense of community belonging are more likely to perceive their mental health positively. Still, it is important to understand that a myriad of intersecting factors can have a significant effect, and this may be primarily seen only in certain populations Footnote 238 . Meaningful connections and support systems can act as a buffer against the stress and challenges of an adjustment, fostering a sense of belonging and acceptance, but these should not be considered determining factors given the other structural determinants of integration Footnote 237 .
Enhancing community belonging is one key factor among many for overall well-being. By understanding and addressing barriers such as employment, language, and discrimination, while also promoting social support networks and inclusivity, local community organizations and mainstream institutions help improve environments for immigrants. Immigrant service agencies play a crucial role as the first point of access for newcomers to explore avenues of belonging within their ethnocultural groups Footnote 233 . Programs where newcomers are matched with established community residents provide opportunities for language practice, socialization, and mutual support Footnote 233 . By nurturing social support networks and facilitating connections between recent and long-term members of the community, these initiatives create an environment where newcomers feel welcomed and valued, thus bolstering the process of integration:
We have volunteer-based programs that are community based, so for example, one of our programs is our cultural links program. It’s a matching program that matches newcomers with established Canadians who are their contact in the community … we don’t say “friend,” but you know it is a friend in the community that they can go to practise their English, to talk about their kids and have their children play together … So we’ve been doing different training sessions with our volunteers including one about how to recognize signs and symptoms of mental health [ sic ]. Footnote 233
Support organizations often take a proactive role in strengthening community bonds for immigrants and challenging discriminatory practices, and attempt to address gaps within Canada’s immigration system Footnote 233 . Local community organizations play a crucial role in integrating newcomers and building their sense of community belonging:
I think [community belonging] will come naturally if all other supports are in place.… I don’t think it’ll happen unless all other systems are in place. Footnote 233
Ninety percent of it is [due to] language. Without the language, they can’t become part of the community, and they remain within their small ethnic community, and they don’t step out. So, they are afraid to step out, and the larger community often resents their lack of integration. Footnote 233
Figure 10 shows trends in strong sense of community belonging by recent and long-term immigrants, between 2007 and 2022. Among females, a similar proportion of long-term and recent immigrants reported having a strong sense of community belonging compared to non-immigrants. The proportion of males with a strong sense of community belonging was similar for immigrants and non-immigrants before 2014; since 2014 to 2016, a greater proportion of recent immigrants than of non-immigrants reported a strong sense of community belonging.
There is little evidence of immigration-based inequality in strong sense of community belonging. This aligns with the findings of other studies, and may be influenced by factors such as Canada’s multicultural policies and differing perceptions of community belonging Footnote 239 . In addition, immigrants shape their sense of belonging to Canada through their experiences after arriving, and are particularly influenced by how they perceive acceptance and the opportunities for success in the host country Footnote 239 . Immigrants’ sense of belonging can also vary based on sociodemographic factors like years since immigration, age at immigration, admission category, and population group Footnote 239 .
Figure 10. Trends in strong sense of community belonging by sex/gender and immigrant status, population aged 12 years and older, 2007–2022
| Year | Sex | Category | Prevalence difference | Absolute change (95% CI) | Relative change |
|---|---|---|---|---|---|
| 2007-22 | Male | Non-immigrant (reference) | 0 | - | - |
| 2007-10 | Male | Recent immigrant | -2.7 (-6.8, 1.4) | -8.5 (-14.9, -2.1) | -314 |
| 2011-13 | Male | Recent immigrant | 0.3 (-5.7, 6.2) | ||
| 2014-16 | Male | Recent immigrant | 7.8 (4.5, 11.2) | ||
| 2017-19 | Male | Recent immigrant | 5.5 (2.0, 9.1) | ||
| 2020-22 | Male | Recent immigrant | 5.8 (0.9, 10.7) | ||
| 2007-10 | Male | Long-term immigrant | -1.3 (-3.2, 0.6) | -1.6 (-4.7, 1.5) | -123 |
| 2011-13 | Male | Long-term immigrant | 1.0 (-1.1, 3.1) | ||
| 2014-16 | Male | Long-term immigrant | 2.1 (0, 4.2) | ||
| 2017-19 | Male | Long-term immigrant | 3.1 (1.2, 5.0) | ||
| 2020-22 | Male | Long-term immigrant | 0.3 (-2.1, 2.7) | ||
| 2007-22 | Female | Non-immigrant (reference) | 0 | - | - |
| 2007-10 | Female | Recent immigrant | -2.4 (-6.2, 1.5) | -3.5 (-9.5, 2.5) | -148 |
| 2011-13 | Female | Recent immigrant | -1.9 (-7.1, 3.4) | ||
| 2014-16 | Female | Recent immigrant | 0.8 (-3.7, 5.2) | ||
| 2017-19 | Female | Recent immigrant | 0.9 (-3.6, 5.4) | ||
| 2020-22 | Female | Recent immigrant | 1.1 (-3.5, 5.8) | ||
| 2007-10 | Female | Long-term immigrant | 0.3 (-1.3, 2.0) | -2.2 (-5.0, 0.6) | -685 |
| 2011-13 | Female | Long-term immigrant | -0.4 (-2.4, 1.6) | ||
| 2014-16 | Female | Long-term immigrant | 0.4 (-1.5, 2.3) | ||
| 2017-19 | Female | Long-term immigrant | 2.3 (0.4, 4.3) | ||
| 2020-22 | Female | Long-term immigrant | 2.6 (0.3, 4.8) |
Abbreviations: CI, confidence interval; PD, prevalence difference; CCHS, Canadian Community Health Survey.
Notes:
Strong sense of community belonging: percent of the population who reported their sense of belonging to their community as “very strong” or “strong” (vs. “weak” or “very weak”). Negative values of the prevalence differences (PDs) indicate absolute inequality in strong sense of belonging over the full time series. A value of 0 indicates that no difference exists between groups on that mental health outcome at a given time point. Changes in inequality are expressed in both absolute and relative scales between only the first and last time periods.
Absolute change calculation: (PD in 2007–2010)−(PD in 2020–2022).
Relative (%) change calculation: 100×[(PD in 2007–2010)−(PD in 2020–2022)/(PD in 2007–2010)].
Absolute and percent change interpretation: positive values indicate an increasing trend in immigration-related inequalities in strong sense of community belonging, negative values indicate a decreasing inequality trend.
Immigrant status is based on respondents reporting that they are landed immigrants/non-permanent residents or non-immigrants (Canadian born).
Data are from annual waves of the Canadian Community Health Survey; population sample is aged 12+ years; estimates age-standardized to the 2016 Canadian census population using 5-year age intervals. Caution is warranted when comparing estimates from cycles prior to 2015 and for data released 2022. We do not exclude the possibility that trends observed may have been influenced by different methodologies used in the CCHS, including a new sample design in 2015.
For more information on data and analysis considerations, refer to https://health-infobase.canada.ca/mental-health/inequalities/technical-notes.html . Inequality trends for other mental health outcomes (e.g., suicidality, depressive symptomatology, life stress) are shown in the accompanying online data tool at https://health-infobase.canada.ca/mental-health/inequalities/data-tool.html .
Social Supports for 2SLGBTQI+ Communities
Networks of support are critical to the mental health of those with intersecting social identities who might otherwise experience social isolation due to systemic and structural barriers (for example, discrimination based on 2SLGBTQI+ identity, ethnoracial identity, and recency of immigration). Social support networks provide a nurturing environment where individuals can find a sense of community, acceptance, and belonging form one of the most significant sources of support for 2SLGBTQI+ newcomers and refugees Footnote 228 . One study in our literature review focused on the experiences of 2SLGBTQI+ newcomers who described how community rooms (where newcomers can drop in to socialize and seek assistance in integrating into Canadian culture or receive employment support) served as innovative and crucial resources to counter loneliness and depression Footnote 228 . These safe spaces allowed individuals to connect with others, share experiences, and find solace in knowing they were not alone Footnote 228 .
Community participation emerges as a vital component of overall well-being, particularly for 2SLGBTQI+ individuals with mental health diagnoses Footnote 240 . The support groups encourage empowerment and help to build resilience, which is essential given the higher rates of discrimination and violence 2SLGBTQI+ individuals experience. Participants in the research with lesbian, gay, bisexual, trans, and queer people with diagnosed schizophrenia and bipolar disorder described how social support groups provided them with the tools to reclaim parts of themselves that were affected by discrimination, helping to rebuild their self-esteem and regain a sense of identity and purpose Footnote 240 .
The value of support groups lies not only in the education and resources they offer but also in the power of being able to share experiences and build upon each other’s stories, which fosters a collective sense of strength and resilience Footnote 240 . As attendees contribute to the narrative, they find a deeper connection to their community and a sense of belonging in their shared history:
It gives people back little pieces of what’s been stolen through a journey of discrimination. Sometimes that’s self-esteem and sometimes that’s education that the [support group] speakers bring. And that really comes through discussion among each other, stories that build upon stories so that people feel stronger in their own narratives. And a sense of place, a sense of belonging in a community and in a history. Footnote 240
Recognizing and fostering social support groups can help significantly reduce mental health disparities and enhance the overall quality of life for 2SLGBTQI + individuals. Such environments empower individuals, providing them with the support, validation, and resources needed to navigate the challenges of social isolation, discrimination, and mental health concerns.
Analyses of CCHS data showed an overall increasing trend in the percentage of the population reporting a strong sense of community belonging between 2007 and 2022. Over this period, gay, lesbian, and bisexual individuals consistently reported lower sense of community belonging than those identifying as heterosexual (Figure 9.A). Among females, the gap was most pronounced between bisexual and heterosexual individuals. Over time, sexual orientation-related inequalities in strong sense of community belonging among females widened by 8.4 and 6.9 percentage points for lesbian and bisexual women versus heterosexual women, respectively. Among males, the gap widened by 5.6 and 5.0 percentage points for gay and bisexual men versus heterosexual men, respectively. None of the sexual orientation-related inequality changes were statistically significant. However, findings should be interpreted with caution due to high variability in the data.
Figure 11. Trends in strong sense of community belonging by sex/gender and sexual orientation, population aged 18–59 years, 2007–2022
| Year | Sex | Category | Prevalence Difference | Absolute Change (95% CI) | Relative Change |
|---|---|---|---|---|---|
| 2007-22 | Male | Heterosexual (reference) | 0 | - | - |
| 2007-10 | Male | Gay/Lesbian | -1.3 (-6.4, 3.8) | 5.6 (-1.7, 12.9) | 422 |
| 2011-13 | Male | Gay/Lesbian | -5.3 (-11.0, 0.2) | ||
| 2014-16 | Male | Gay/Lesbian | -6.2 (-12.0, -0.5) | ||
| 2017-19 | Male | Gay/Lesbian | -7.8 (-13.0, -2.5) | ||
| 2020-22 | Male | Gay/Lesbian | -6.9 (-12.0, -1.7) | ||
| 2007-10 | Male | Bisexual | -4.5 (-12.0, 2.6) | 5.0 (-5.3, 15.4) | 112 |
| 2011-13 | Male | Bisexual | -6.7 (-15.0, 1.7) | ||
| 2014-16 | Male | Bisexual | -7.6 (-15.0, -0.6) | ||
| 2017-19 | Male | Bisexual | -10.0 (-18.0, -2.5) | ||
| 2020-22 | Male | Bisexual | -9.5 (-17.0, -2.0) | ||
| 2007-22 | Female | Heterosexual (reference) | 0 | - | - |
| 2007-10 | Female | Gay/Lesbian | -2.3 (-7.4, 2.8) | 8.4 (0.2, 16.5) | 366 |
| 2011-13 | Female | Gay/Lesbian | -5.7 (-12.0, 0.6) | ||
| 2014-16 | Female | Gay/Lesbian | -7.9 (-14.0, -1.4) | ||
| 2017-19 | Female | Gay/Lesbian | -3.6 (-9.1, 2.0) | ||
| 2020-22 | Female | Gay/Lesbian | -11.0 (-17.0, -4.3) | ||
| 2007-10 | Female | Bisexual | -6.1 (-12.0, -0.5) | 6.9 (-1.2, 15.1) | 114 |
| 2011-13 | Female | Bisexual | -8.1 (-15.0, -1.1) | ||
| 2014-16 | Female | Bisexual | -6.6 (-12.0, -1.4) | ||
| 2017-19 | Female | Bisexual | -11.0 (-15.0, -5.8) | ||
| 2020-22 | Female | Bisexual | -13.0 (-19.0, -7.2) |
Abbreviations: CI, confidence interval; PD, prevalence differences; CCHS, the Canadian Community Health Survey.
Notes:
Strong sense of community belonging: percent of the population who reported their sense of belonging to their community as “very strong” or “strong” (vs. “weak” or “very weak”). Negative value PDs indicate absolute sexual minority vs. heterosexual inequality in strong sense of belonging over the full time series. A value of 0 indicates that no difference exists between groups on that mental health outcome at a given time point. Changes in inequality are expressed in both absolute and relative scales between only the first and last time periods.
Absolute change calculation: (PD in 2007–2010)−(PD in 2020–2021).
Relative (%) change calculation: 100×[(PD in 2007–2010)−(PD in 2020–2022)/(PD in 2007–2010)].
Absolute and relative (%) change interpretation: positive values indicate an increasing trend in sexual orientation inequalities in strong sense of community belonging, negative values indicate a decreasing inequality trend.
Respondents reported on sexual orientation by choosing from the following predetermined categories: “heterosexual,” “gay or lesbian,” and “bisexual.” From 2019 to 2021, the Canadian Community Health Survey (CCHS) included pansexual individuals in the bisexual category but was removed in 2022.
Data are from annual waves of the CCHS; population sample is aged 18–59 years due to a restriction on age of respondents asked the sexual orientation question prior to 2015; estimates age-standardized to the 2016 Canadian census population using 5-year age intervals. Caution is warranted when comparing estimates from cycles prior to 2015 and for data released 2022. We do not exclude the possibility that trends observed may have been influenced by different methodologies used in the CCHS, including a new sample design in 2015.
For more information on data and analysis considerations, refer to https://health-infobase.canada.ca/mental-health/inequalities/technical-notes.html . Inequality trends for other mental health outcomes (e.g., suicidality, depressive symptomatology, life stress) are shown in the accompanying online data tool at https://health-infobase.canada.ca/mental-health/inequalities/data-tool.html .
Impacts of Climate Change on Sense of Community Belonging for Indigenous People
Climate change exerts a profound effect on mental health, giving rise to heightened levels of anxiety, often called ecoanxiety or climate anxiety, a form of distress stemming from environmental crises Footnote 329 . Individuals may grapple with the fear of an uncertain future, loss of biodiversity, and looming threats Footnote 329 . The devastation wrought by climate-related disasters can result in ecogrief (or climate grief), a deep sense of sadness, helplessness, and mourning for environmental losses Footnote 329 . These interconnected factors make it increasingly crucial to address climate change as a determinant of mental health.
While the health outcomes of climatic variability and environmental changes have been well-documented in terms of food and water quality, waterborne and vectorborne diseases, and increased injury and death as a result of extreme weather events, including heat waves, storms, floods, drought, and wildfires Footnote 241 Footnote 242 Footnote 243 , the relationship between climate change and emotional, mental health, and well-being is only now becoming apparent Footnote 244 .
Although the effects of climate change are exacerbating health and socioeconomic inequities across Canada, people who depend on local ecosystems and natural resources, including Indigenous People living in rural communities, are particularly vulnerable to the direct and indirect impacts Footnote 238 Footnote 245 . The pathways through which climate change threatens mental health and wellness include the following cross-cutting themes: land attachment and ways of life, cultural loss and continuity, and food insecurity.
Through a rapid literature review, we identified 7 studies that focused on climate change and mental health and wellness in Rigolet, an Inuit community in the Nunatsiavut region of Newfoundland and Labrador Footnote 244 Footnote 246 Footnote 247 Footnote 248 Footnote 249 , and 5 studies in Inuit communities in Nunavut Footnote 250 Footnote 251 Footnote 252 Footnote 253 Footnote 254 .
For Inuit, the land is deeply connected to individual and community identity through a sense of reliance on the land for livelihood and culture:
It’s who and what we are, connecting to the land, to the environment, to the sea, to nature, to everything that’s around us... it’s a part of our culture. It’s what wakes you up in the morning to get you going, to be on the land, to be able to participate, to share, to love, to protect it, to look out for all of those things. Footnote 247
Engaging in land-based activities not only reinforces this connection, but is vital to Inuit mental and emotional wellness:
For some people, going out on the land is just as good as sitting down in a counselling session—no need for words, the air and the land takes a lot of your feelings away and replaces the negative energy with the positive energy of nature. Footnote 244
The Inuit culture comprises important traditions, practices, and knowledge that connects individuals to their ancestors, community, and identity and fosters a strong sense of belonging:
[Being on the land] is important to me because … I've always been out on the land with my family, so one thing why it’s important is that it’s almost like tradition to do things as a family out. It’s also important to me because it’s part of my culture, and it’s also important because the way you feel when you’re out on the land. It feels good. Footnote 255
Changes to the land can elicit place-based distress if connection to the land and ancestors and continuity of traditions is threatened, straining the ability for Inuit to maintain connection with their communities and the ability to foster a strong sense of belonging Footnote 244 Footnote 249 Footnote 253 Footnote 255 .
Climate change impacts mental health by restricting access to the land and altering the land’s resources, thereby depriving communities from a culturally significant way of life and of nurturing individual and community well-being Footnote 244 Footnote 250 Footnote 251 Footnote 252 Footnote 253 Footnote 256 Footnote 257 Footnote 258 . Animal habitats, fishing areas, and community infrastructures have been degraded or destroyed, creating additional barriers to hunting and harvesting country and traditional foods, affecting Traditional Knowledge transfer, and exacerbating existing food insecurity Footnote 252 Footnote 254 Footnote 258 .
Hunting and harvesting of country foods is part of the Inuit Traditional Knowledge:
[Teaching my 5-year-old son to harvest country food is important because] he could pass it down to his kids too when he has kids Footnote 252 .
Hunting is also part of the practice of sharing and building community bonds:
For this community—[and for] a lot of hunters—a good, successful hunt means distributing to the community and sharing information about it over the local radio, or [to] family members within the community Footnote 251 .
Box 4.4: Community Belonging and Cultural Connection for First Nations living off reserve, Inuit, and Métis
Community, kinship, connectedness, and social cohesion are at the core of Indigenous cultures, and studies have shown that social connectedness is associated with positive mental health outcomes for Indigenous Peoples Footnote 259 Footnote 260 Footnote 261 Footnote 262 . Social cohesion translates into reciprocal relationships that can provide support in times of need, which reduces the physiological response to stress, providing a protective effect Footnote 263 .
Using data from the CCHS from 2009 to 2022, we examined trends in life satisfaction for the intersection between Indigenous identity and sense of community belonging. During this period, First Nations living off reserve, Inuit, and Métis respondents who reported a weak sense of community belonging consistently reported lower levels of mean life satisfaction compared to non-Indigenous respondents reporting a weak sense of community belonging. This disparity was less pronounced but nevertheless increased over time, among First Nations living off reserve, Inuit, and Métis respondents who reported a strong sense of community belonging compared to their non-Indigenous counterparts. The increase in disparity was especially noticeable during the COVID-19 pandemic (2020–2022).
Indigenous cultures, which provide the foundation for individual and collective identity, are at the core of this sense of connectedness or belonging Footnote 264 . Past and ongoing colonial structures in Canada have systematically attempted to erode Indigenous cultures through the establishment of the Indian Act , the residential school system, the Sixties Scoop, and other laws, policies, ideologies, and initiatives that had the goal of suppressing the use of Indigenous languages, cultural practices, and traditions Footnote 179 Footnote 265 .
This systematic effort to suppress Indigenous cultures and the resulting intergenerational trauma has contributed to the loss of social cohesion Footnote 172 Footnote 187 Footnote 266 . While the effects of the erosion of culture and community cohesion vary, in many Indigenous communities the historical trauma and pain related to loss of cultural identity have manifested as problems associated with substance abuse Footnote 267 Footnote 268 .
Evidence shows that restoring traditional healing and other cultural practices that enforce Indigenous identities can help address many of the root causes of substance abuse in Indigenous communities Footnote 269 . Initiatives that reinforce cultural affiliation, community involvement, and traditional practices have been associated with lower rates of substance abuse Footnote 270 Footnote 271 .
While interventions that foster Indigenous cultures have been shown to provide a useful tool for addressing substance abuse, other supports must also be in place, particularly those that address the root causes of trauma and the erosion of social cohesion. Working to address the social determinants of Indigenous mental wellness is a shared responsibility that requires concerted intersectoral action.
4.1 .4 Access, Quality, and Use of Health Care Services
Access to health care services is a well-recognized social determinant of health and despite the universal health care system in Canada, some groups face difficulties in accessing services. For instance, immigrants in Canada experience access barriers to healthcare, including socioeconomic, communication and cultural factors. In addition, Indigenous Peoples face inequitable access to health services in comparison to the general Canadian population due to factors such as geographical constraints, lack of health human resources, discrimination and a lack of culturally safe services.
Systems of power shape investment in and distribution of social and health services across communities, as well as the mandate, scope, quality and safety of health and social services Footnote 54 . Qualitative studies that were reviewed provided several examples of the ways in which systems of power influence access, quality, safety and use of social and health care services. Among the 67 Canadian articles examined, 42 addressed access to care, and included a variety of populations and communities, including sexual and gender minorities, youth, women with postpartum depression, populations experiencing homelessness, racialized communities, people who inject drugs, and individuals with severe mental illness.
Three prominent areas related to access and quality of care emerged from the literature and will be discussed, including 1) availability and barriers to care; 2) safety and quality of mental health care; 3) access to treatment.
Availability and Barriers to Care
The availability of and barriers to accessing mental health care and treatment was a recurring theme in our review of qualitative studies. Structural barriers, including the lack of public health insurance coverage for treatment of mental health conditions by non-physicians in all provinces and territories and access to employer paid supplemental insurance, contribute to and sustain inequities in mental health care access among different population groups. It is estimated that one third of the working population in Canada do not have access to this type of private insurance, which can be used for mental health services including psychologists, psychotherapists and social workers. For those who do have coverage, inadequate coverage present further difficulties Footnote 272 Footnote 273 .
For individuals in need of care, additional barriers include challenges finding a family physician, who is often the first point of contact for subsequent referrals, limited availability of and not enough specialists, long wait times to see specialists, and short appointment durations Footnote 240 Footnote 274 Footnote 275 Footnote 276 Footnote 277 Footnote 278 Footnote 279 .
Increasing costs of living are resulting in individuals cutting back on health-related expenses, which can lead to worsening mental health Footnote 267 . Acute care services, such as hospital treatment and primary care physicians, are covered by public health insurance plans, but many other mental health services—counselling, psychotherapy, social work case management, addiction and eating disorder treatments, among others—are not publicly funded and are unaffordable for many Footnote 267 . Charities and non-profit organizations help in providing to some services free of charge, with the overall demand for these services growing Footnote 267 . Socioeconomic limitations faced by individuals, lack of access to private health insurance, and insufficient publicly funded mental health services exacerbate mental health disparities for those most in need of care.
For individuals in need of care, additional barriers include challenges finding a family physician, who is often the first point of contact for subsequent referrals, limited availability of and not enough specialists, long wait times to see specialists, and short appointment durations Footnote 240 Footnote 274 Footnote 275 Footnote 276 Footnote 277 Footnote 278 Footnote 279 .
Indigenous Peoples, particularly those living in rural, remote and northern communities, face specific barriers accessing health services. Many of these communities face critical shortages of healthcare personnel, relying on non-resident health professionals who fly periodically to these areas to provide services. This leads to long wait times, resulting in delayed diagnoses, disrupting continuity of care, and reducing the effectiveness of health services. As a result, many patients are transported to urban centers in the south, often leaving families and support networks behind during what often requires a series of periodic back and forth trips Footnote 280 .
In terms of access to publicly funded services for mental health or substance use issues, in our review of qualitative literature, individuals with mental health and substance use issues found it particularly difficult to access primary care. In addition, newcomer status, history of substance use, poverty, homelessness and past criminal record were all perceived as barriers for access to physician care. The need for increased provider paperwork placed an additional barrier for individuals that received financial support for disability or other types of social assistance Footnote 278 .
Models of health care funding and associated rules, such as the practice of discussing one health condition per visit when seeing a doctor, places stress on both health care providers and patients. Patients found consultation times brief, leading them to feel rushed during appointments Footnote 278 Footnote 281 . Meanwhile, service providers also felt that the appointment length was not adequate to address the health care needs of patients, particularly those with complex needs Footnote 278 .
In addition, the ongoing problem of long wait times to see a specialist, such as a psychiatrist or an Eating Disorder Specialist and limited or no availability, continues to be a significant barrier to seeking care. For example, participants expressed there were more services for those with drug and alcohol use than for those seeking treatment for eating disorders, even though they might be privately paid Footnote 276 . Both youth experiencing disordered eating and service providers alike found it difficult to find services to provide assistance for body image and food concerns Footnote 276 . One service provider stated:
“I can’t think of one place that you might be able to go to for an eating disorder, [but] I can think of at least five or six places just off the top of my head for drug and alcohol addictions.” – Employee of an [Indigenous] youth organization Footnote 276
Even though there are potentially more services available for addiction treatments, long wait times and limited hours of operation place a significant barrier to receiving treatment. Further, many services are privately delivered, and therefore only accessible to those with financial means. Delays in receiving treatment can exacerbate health related problems, for instance, one study found that services had restricted or daytime operating hours at needle exchange centres and pharmacies, which sometimes resulted in unsafe needle sharing practices Footnote 277 . One participant shared their experience:
“The pharmacy isn’t open 24 hours and….the biggest necessity for clean needles is actually during…hours which aren’t regular business hours….so there was times that I found myself having to use someone else’s syringes and those were times when you know the pharmacies were closed and the needle exchange was closed.” -Study participant using drug use support services Footnote 277
In the same study, a participant left Prince Edward Island to go to New Brunswick for treatment due to lengthy wait times Footnote 277 . Another participant shared:
[The Treatment Facility staff] ask you at some point, “Do you wish to be placed on the methadone list?” You say, “Yes.” They say, “Well, great, we’ll probably talk to you in about a year’s time.” -Study participant looking for addiction treatment Footnote 277
Long wait times were a common difficulty. One study participant recounted:
“I was getting abused, one time. When I phoned [transient housing], they told me to call back... they’re saying ‘phone me back in a couple weeks and we might have an opening’” Footnote 275 .
Location can also play a role in the availability of care. Rural areas often have more limited services in comparison to urban areas. For example, a study with participants in rural regions found that specialized care for drug use and pain management was not available and was only accessible in urban centres. Rural areas often had access to only one physician who could provide them with medical support Footnote 279 .
Intersecting social locations and identities further hindered and posed unique barriers to accessing care. Youth faced challenges in accessing injection cessation care due to various structural, social and environmental barriers, including long wait times, discrimination based on race, sexuality and gender, lack of social support and housing provisions Footnote 282 . Youth with disordered eating felt there was a shortage of infrastructure to receive support Footnote 276 . Lone mothers faced challenges of finding affordable childcare, expensive costs of transportation and feelings of stigmatization for receiving help Footnote 283 . Regarding 2SLGBTQI+ populations, service providers felt that there were not enough services that took sexual orientation and gender identity into consideration Footnote 240 . One service provider shared:
“I don’t think there’s enough types of services to help people from our communities, mental health community, the [lesbian, gay, bisexual, and transgender] community. God forbid if you have both labels, you’re in real big trouble” -Service provider Footnote 240
Another study participant found it difficult to find services for racialized 2SLGBTQI+ individuals. This participant described how this affected his participation in using mental health services:
“I think I would probably be a lot more interested in going to an organization like that, that was inclusive of gay people and people of colour. I think that would be a wonderful organization...I would probably want to reach out a lot more and maybe develop more platonic friendships”- Study participant Footnote 240
Overall, different population groups and individuals with intersecting identities are experiencing challenges in accessing mental health care due to various structural, social and environmental barriers. Increased access and availability to mental health services with an equity plan to target different affected population groups would help improve mental health among Canadians.
Safety in Accessing and Quality of Mental Health Care Services
Beyond barriers to care in terms of availability, many qualitative studies reported that sexism, heterosexism, homophobia, transphobia, racism, and stigma related to mental illness and substance use affected access to mental health care Footnote 240 Footnote 283 Footnote 284 Footnote 285 Footnote 286 Footnote 287 Footnote 288 . The dominance of psychiatric and biomedical perspectives often feel restrictive to individuals and do not recognize life histories, trajectories, and individual experiences that affect mental health and wellness.
Pathologizing narratives of deviance, individualizing blame, and ideological oppression continue to affect those experiencing psychological difficulty, with very little emphasis on acknowledging the larger social, political, and economic factors that impact mental health and wellness.
Safety in Accessing Mental Health Care Services
The concept of safety in accessing care for mental health was significant for numerous people and was most pronounced among individuals experiencing overlapping marginalized identities. Gender-based physical and psychological violence contributed to and exacerbated mental health struggles for many women and 2SLGBTQI+ individuals trying to access care.
For example, the effects of intimate partner and sexual violence have been shown to be amplified by health systems, health care providers, and members of law enforcement, who perpetuated gender discrimination, particularly for those who use substances. In Iris et al.’s study of women living in poverty and struggling with substance use during pregnancy, one participant, who had been sexually assaulted and was being criminalized for suspected substance use, explains Footnote 288 :
“When I came in, they didn’t want to check me right away. I was bleeding, I was in a lot of pain, I was crying, but they just said ‘No, the officers are here.’ And the cops kept harassing me, saying ‘Oh, were you using drugs? You deserve…’ well not to get raped, but they were basically saying ‘oh, you asked for it.’ And all I kept saying was that I wanted to get checked for the baby, and they kept saying, ‘You have to wait, the officers want to talk to you’ and I kept saying ‘Check my baby, I’ll talk to them later,’ right? I was really upset – I just got raped, and they’re trying to question me?” Footnote 288
For some women, their experience of intimate partner violence and need for medical attention for self-harm or suicidal ideation was met with mistreatment and hostility by health care providers, intensifying their mental distress. Health care providers’ “dehumanization, invalidation, and lack of empathy” was particularly troubling for women already experiencing crisis, causing further harm Footnote 289 . As one participant describes in Taylor’s study of women who sought help for suicidality after experiencing intimate partner violence:
“You can go [to the emergency department] and suffer worse than if you were being abused by your partner because you leave there feeling like you are worthless. Even if you tell them you were suicidal, it is not taken seriously. They almost refuse to treat you. They refuse to talk to you. You are just worthless.… You can come out of [the hospital] feeling three times worse than when you go in with a crisis... because [the health care providers] are too judgmental” Footnote 289
For some street-involved women experiencing severe poverty, accessing care and treatment felt judgmental and individuals were met with disdain, which subsequently led to delayed care seeking for medical and mental health–related issues Footnote 284 Footnote 287 .
While women-only services addressed some safety concerns and offered a positive environment with a variety of practitioners, services were often limited to pregnancy and gynecological concerns. One critique of this approach emphasized biomedicine’s tendency to restrict care of women to their reproductive role. This neglected women’s needs throughout the life course, particularly for those who are socially isolated and requiring different types of mental health and medical services. As one described:
“Nobody talks about women getting older. There is nothing for us. We don’t matter any more. Older women need more services. When I was 20, I didn’t need health care. Now I have nowhere to go.” Footnote 284
For 2SLGBTQI+ individuals, lack of gender and sexuality–affirming options for mental health care contributed to a lack of safety. Care and therapeutic strategies that do not recognize the larger context of heterosexism, structural homophobia, and transphobia can erase the lived realities of 2SLGBTQI+ people, for whom judgment can often be accompanied by violence Footnote 240 Footnote 286 .
“I don’t think [mental health agencies] are as welcoming as they are to the heterosexual population. From personal experience, just the looks, and the attitude, and the body language, and just all of it. I think it’s disgusting” Footnote 240 .
Although some strides have been achieved in urban centres, where 2SLGBTQI+-positive health facilities are available, many people experience discrimination in care due to their sexual orientation and gender presentation, care providers’ assumptions of heterosexuality as the norm, questioning of gender, and a lack of acceptance of the diverse needs of 2SLGBTQI+ people. Feeling judged, belittled, and uncomfortable can leave individuals feeling left out and cause them to end treatment sooner Footnote 209 Footnote 212 Footnote 290 .
Acceptance of gender diversity was a critical element in perceived safety of care. For transgender individuals in particular, confusion around gender identity was directly related to safety. In Lyons et al.’s study of transgender individuals’ experiences in residential addiction treatment facilities, one participant describes Footnote 212 :
“It was really difficult. I went there and … when I got there they had no idea I was transgender. … They didn’t know how to deal with it.” Footnote 212
In this same study some, acceptance and respect of gender identity through providing access to gender-appropriate treatment groups with appropriate gender groups in treatment and housing led to increased feelings of safety and inclusion Footnote 212 .
Cultural safety is a concept that aims to provide a safe and respectful environment for Indigenous Peoples to receive healthcare services. It is a process of recognizing and addressing power imbalances between healthcare providers and Indigenous Peoples, and creating an environment where Indigenous Peoples feel respected and valued. This includes acknowledging the historical and ongoing trauma experienced by Indigenous Peoples, and the impact it has on their health and well-being. It also involves understanding and respecting Indigenous Peoples’ cultural beliefs, values, and practices, and incorporating them into healthcare services Footnote 291 . Cultural safety is essential for Indigenous Peoples to access healthcare services without fear of discrimination or racism, and to receive care that is appropriate and respectful of their unique needs and experiences Footnote 292 .
Quality of Care Received
The quality of care received for treatment of mental health was another important factor related to access. At a structural level, barriers to achieving quality of care for people living with mental health and substance use issues, include a lack of coordination and integration that requires sufficient interaction and collaboration between health care institutions and health care providers Footnote 278 Footnote 293 and other potential stakeholders (e.g., social work) Other system level difficulties are related to silos of care, the dominance of psychiatric and pharmaceutical treatment for mental health Footnote 285 Footnote 286 , and inadequate training and insufficient numbers of health care providers to address substance use and addictions Footnote 277 .
For those individuals who are precariously housed or experiencing homelessness and those experiencing poverty, selective care for physical conditions, mistreatment, overprescribing of medication and poor quality or denial of care was a common experience Footnote 294 . A study that explored how accessible health care services are for individuals who are experiencing homelessness through interviews of their experiences had one participant described the following:
“I have [posttraumatic stress disorder] and the doctor said he didn’t like my disposition. You don’t have to like my disposition, I’m not here to make friends with you. You tell [the doctor] you have a drug problem and a mental problem, he won’t help you with your mental problem. He’ll be like, “You have to quit the drugs first.” How, if I’m mentally unstable, am I going to quit drugs? I’m using drugs to try to cope.” Footnote 294
Another important aspect of the quality of care received is its relevance to individuals’ lives and experiences. In terms of mental health, relevance pertains to care that recognizes cultural diversity and sees mental health and wellness more broadly, beyond biomedical approaches and psychiatric definitions. Care was perceived to be more relevant persons seeking care if it was community based, grassroots, holistic, culturally appropriate, gender-equitable and non-racist Footnote 184 Footnote 188 Footnote 283 Footnote 285 Footnote 295 Footnote 296 .
Many studies described the need for culturally relevant and responsive mental health supports with respect for diverse customs, values, and beliefs Footnote 184 Footnote 282 Footnote 285 . Auger’s study discusses Métis people’s difficulties accessing and navigating the Western health care system Footnote 184 . Participants often spoke about the lack of culturally safe mental health providers and historical trauma rooted within health care experiences:
“My grandmother was hospitalized, my Métis grandmother. She was given electric shocks. She was so heavily medicated. I was terrified of medication all my life because of seeing her so heavily medicated” Footnote 184
Participants spoke about the importance of both Western and traditional healing for themselves:
“I do see a clinical counsellor every couple of weeks, but I don’t see that as being more helpful than going to the beading group, than going to Métis Night at the Friendship Centre” Footnote 184
Despite seeing the value of both forms of healing, participants often spoke about identified gaps in programming, illustrating the importance of Métis-specific health programs and services:
“I want to see Métis people included in conversations about Aboriginal mental health, about Aboriginal child and youth mental health. I think that we need to not be footnotes anymore—if we’re even footnotes. Oftentimes, we don’t even make it into the report or onto the program curriculum or things like that.” Footnote 184
If and when care was available and accessible, implicit bias and lack of diversity among mental health professionals affected treatment. Studies have shown that there is a dire need for providers that understand mental health and wellness more holistically, including how religion, culture, family, intergenerational expectations, language, and tradition impact mental health and wellness Footnote 188 Footnote 285 Footnote 296 .
“…Psychiatrists who deal especially with youth. The thing is that there are not many of them… Also, the lack South Asian mental health professionals… The Western approach to mental health is very, very different from the South Asian approach to mental health. One is not better. It’s just very different… There is a huge emphasis on meds… Also, a big difference between Western and South Asian mental health is that there is more emphasis on religion in South Asian mental health treatment… Western health is very secular and very like you need to do things on your own.” Footnote 285
In instances where relevant services were identified, cultural barriers at the point of service delivery tended to limit the utilization of such supports for study with African immigrant parents on factors influencing their children’s mental health Footnote 296 . Distrust of the health care system was also prevalent, which served to discourage contact with professional mental health care providers when the need to do so arose. Coming largely from cultural backgrounds that stigmatize mental illness, the tendency of service providers to document service utilization was a source of distrust. Thus, out of fear of being documented and stigmatized, African immigrant parents were hesitant to access counselling services and other mental health supports for their children Footnote 296 .
Positive quality of care was experienced for participants in some studies, where treatment was perceived to increase social connectedness, acceptance and access to community. Supervised (or safe) consumption sites, overdose prevention sites, and safe injection sites are settings that offer clean and safe environments for using substances Footnote 287 Footnote 295 Footnote 297 Footnote 298 . Strict rules related to violence and aggression and information about the safety of the drug supply further enhanced the positive contribution of using substances in a harm reduction environment Footnote 287 .
“Drug use is a very, very solitary sport, and it’s fraught with despair, isolationism, and desolation—and real darkness. And when you’re using a safe injection site, you’re using in the context, in the social context, so it breaks all that” Footnote 287
Supervised consumption sites also protect people from criminalization as they provide a place for safe drug use without fear of getting arrested because of their homelessness and drug use Footnote 287 :
“From a legal standpoint, I don’t feel like I’m going to get in trouble, so I’m not rushed. It allows me to make better decisions about my usage.” Footnote 287
While another positive aspect of the supervised consumption sites is the ability to access a wider range of health services, such as primary care, treatment for addictions, psychiatry, and sexual health services Footnote 287 , adopting a more holistic understanding of substance use may be more helpful. Adequate and appropriate care that addresses child abuse, foster care, and trauma are essential Footnote 299 .
Access to treatment – stigmatization due to substance use and serious mental illness
Another significant factor affecting access to care were stigma experienced by people who use drugs and/or those with serious mental illnesses. The drivers of stigma related to substance use are beliefs that “substance use is moral failure, rather than a real illness, and that people are to blame for their condition; that people who use substances could ‘choose to stop’; and that people who use substances are dangerous and reckless” Footnote 300 .
There were several experiences of stigma based on substance use in the qualitative literature search. Stigma was experienced in various settings, including different treatment settings such as hospitals, medical services and residential treatment settings by service providers and health care practitioners. It was also reported in personal settings such as at home by family members.
Participants reported stigmatizing experiences because of their race or ethnicity, appearance, and substance use. They also reported feeling that they were treated differently than others based on health care providers’ mistrust, lack of compassion, and more aggressive treatment Footnote 275 . Participants felt that their drug use was not accepted by the general public and that they were treated with suspicion by their family and friends Footnote 275 . One participant recounted:
“Even my own family... they all know I’m a junkie, like I don’t hide the fact... they’re all afraid that I’m gonna rip them off or steal their money” Footnote 275 .
Experiences of stigma as a result of substance use affected individuals’ access to care. One person described providers focusing solely on their addiction and, as a result, feeling like that had to lie to access care:
“They [nurses] talk to you, all condescending, like the only health issue that you have or ever will have has to be an addiction-related thing. I mean, I actually went in and refused to say that I did drugs, and hid it because I felt like they were looking at nothing else in my health except something that was addiction related... I mean, if you are lying you’re obviously not going to receive the services you need, right? And unfortunately with most of the health care I’ve accessed I’ve felt like I have to lie; I had to make up that I was a different person so I could access care” Footnote 284 .
Another participant in a study felt that their status as a person who injects drugs compromised their receiving acute medical services Footnote 277 . An example of this was when they waited over 8 hours in hospital for a drug-related issue, and overhead staff at the hospital saying:
“[He] is just a drug addict or a narcotics user … just put him in a corner until later.” Footnote 277 .
Another study found that participants felt as though primary care providers did not want to engage in conversations related to mental health and substance use issues. The health care provider would explicitly or implicitly say that these were outside of their scope of practice and would not discuss these issues. The participants felt this was related to lack of knowledge on these topics Footnote 278 .
While withholding information about drug use could mean that some health concerns are not addressed, female study participants considered this approach to be better if they wanted to be treated with respect and avoid “feeling less than human in their [health care providers’] eyes.” Footnote 284 .
Different population groups recounted experiences of stigma including women. Women described feeling stigmatized as an addict or not being recognized as “real people” by health care providers as they lacked control of the information shared through their medical records, such as address and substance use Footnote 284 . They reported being lectured to by health care providers about drug use and instances where health care providers ignored their questions. They reported feeling punished for advocating for themselves or for questioning the practices of health care providers Footnote 284 .
Women also experienced double standards when accessing overdose prevention sites Footnote 295 . Compared to men, women were expected to behave better, care for others, tidy up, and consume drugs faster. They were also expected to serve as caretakers for men while still having to generate income to purchase drug Footnote 295 . One participant recounted:
“We’re just held to a higher standard. Yes, we are expected to behave better. We’re expected to not stay as long [at overdose prevention sites]. We’re expected to not sleep on the floor … We’re the money makers and we’re the [care] takers. We take care of the boys and, you know, we are supposed to come in and clean and take one [a male client] with you, because that happens a lot right. You come get your boyfriend or whatever.” Footnote 295
One woman was unable to receive mental health care because of the nature of her diagnosis. She recounted:
“I said ‘I have [dissociative identity disorder]’ and she [health care provider] said, ‘What’s that?’ And I [told] her and she stopped the interview right there and said, ‘We don’t deal with people like you here’…. So I just left and started crying and walked home.” Footnote 278
Another population group that experienced stigma for drug use was based on sexual and gender identity, particularly transgender individuals. Participants in the studies reported feeling isolated, uncomfortable, a lack of understanding of gender identity from the staff and inappropriate comments from staff Footnote 212 . One participant felt that other people’s responses to her transgender identity prevented her from treating her addiction:
“I had a lot of support from the staff, but with the other clients, it was really difficult. I mean everybody’s talking in the whole unit about me …‘cause I’m the only transgender.… I ended up isolating myself and locked in my room 24 hours a day.… It’s like, this isn’t dealing with your addiction.” Footnote 212
Some staff reported that they were unaware of transgender identities and did not know how to respond to them Footnote 212 . A Two-Spirited participant discussed her experience with a counsellor who challenged how someone with this gender identity should act:
“[My counsellor] said that I wasn’t being true to myself because I was not acting like a normal Two-Spirited person would and I would argue with her like, well not argue, but debate with her, how am I supposed to act. Am I supposed to stay here and pop a hip every time? [She was saying you weren’t feminine enough?]. Yeah, it was weird. I just didn’t really like talking about it and … she was rude. She was really, really rude. So yeah, I left.” Footnote 212
Another participant discussed feeling uncomfortable to discuss certain topics due to sexual identity and the social environment. The participant said:
“In the groups I wouldn’t come out and talk about certain things because there were other straight people there. But I know that lesbian and gay people and trans, if they heard me talk about these other things they wouldn’t go ‘oh my god,’ but a straight person would.”- Study participant Footnote 212
These experiences of stigma towards substance use from health care providers and peers make it more difficult to access mental health services. Figure 9 presents inequalities in unmet need for mental health care services based on sex/gender, sexual orientation, household income, level of education, racialized identity, and immigration status. Among individuals who report a need for mental health care services (e.g., counseling, medication), the unmet need indicator measures the percent whose needs were unmet or partially met.
Between 2012 and 2022, individuals identifying as gay or lesbian (LGB) or bisexual, immigrants, and racialized respondents reported higher rates of unmet mental health service needs compared to heterosexual individuals, non-immigrants, and White individuals, respectively. In 2022, females also reported greater levels of unmet need for mental health services than males. Absolute inequalities in unmet needs based on sex/gender and sexual orientation tended to increase over time, while little change was observed on the relative scale.
In contrast, for household income, education level, and immigration status, there was evidence of declining absolute and relative inequality estimates over time. For racialized identity, estimates of relative and absolute inequality significantly decreased between the two time periods (i.e., rates of unmet needs for racialized individuals were 21% or 8.1 percentage points lower compared to White individuals in 2022). Because of the high variability in the data, however, these results should be interpreted with caution.
Figure 12. Inequalities in unmet need for mental health care services, population aged 15 years and older, 2012 and 2022
| Group |
Prevalence difference for unmet need for mental health services (95% CI) |
Absolute change in prevalence difference (95% CI) |
Prevalence ratios for unmet need for mental health services (95% CI) |
Relative change in prevalence ratios (95% CI) |
||
|
2012 |
2022 |
2022 vs. 2012 |
2012 |
2022 |
2022 vs. 2012 |
|
|
Female vs. male ( reference ) |
0.1 (−4.1, 4.3) |
2.1 (0.2, 4.0) |
1.9 (−2.7, 6.6) |
1.00 (0.88, 1.15) |
1.05 (1.00, 1.10) |
1.05 (0.91, 1.20) |
|
Gay/lesbian/bisexual vs. heterosexual ( reference ) |
11.5 (0.9, 22.1) |
18.1 (15.3, 20.9) |
6.6 (−4.4, 17.6) |
1.37 (1.06, 1.76) |
1.46 (1.38, 1.53) |
1.07 (0.88, 1.29) |
|
Lower income (bottom 40%) vs. higher income (top 60%) ( reference ) |
4.5 (0.2, 8.8) |
0.4 (−1.5, 2.3) |
−4.1 (−8.8, 0.6) |
1.15 (1.01, 1.31) |
1.01 (0.96, 1.06) |
0.88 (0.78, 1.00) |
|
University degree vs. less than university degree ( reference ) |
−1.1 (−6.7, 4.5) |
0.6 (−1.3, 2.4) |
1.7 (−4.3, 7.6) |
0.97 (0.81, 1.15) |
101. (0.97, 1.06) |
105. (0.87, 1.27) |
|
Immigrant vs. nonimmigrant ( reference ) |
8.7 (2.5, 14.8) |
6.8 (4.7, 9.0) |
−1.8 (−8.3, 4.7) |
1.29 (1.09, 1.51) |
1.17 (1.12, 1.23) |
0.91 (0.80, 1.04) |
|
Racialized vs. White ( reference ) |
15.5 (7.7, 23.2) |
7.3 (5.2, 9.4) |
−8.1 (−16.2, −0.1) |
1.51 (1.26, 1.80) |
1.19 (1.13, 1.25) |
0.79 (0.70, 0.89) |
Abbreviations: CI, confidence interval; PD, prevalence difference; PR, prevalence ratio.
Notes:
Unmet need for mental health services: among respondents who reported a need for mental health services (including counselling, medication), the proportion (%) who reported that some or all these needs were unmet. Positive values of the prevalence differences (PDs) indicate absolute inequality in unmet need. Prevalence ratio (PR) values above 1.0 indicate relative inequality in unmet need.
Absolute change calculation: (PD in 2022)−(PD in 2012).
Relative (%) change calculation: (PR in 2022)/(PR in 2012).
Absolute and relative (%) change interpretation: Positive values indicate an increasing trend in inequalities in unmet need, negative values indicate a decreasing inequality trend in unmet need.
Data are from the Canadian Community Health Survey – Mental Health (2012) and Mental Health and Access to Care Survey (2022). Population sample is aged 15+ years, living in the 10 provinces; estimates are age-standardized using 2016 Census 5-year age intervals. Further information on data and analysis considerations can be found at https://health-infobase.canada.ca/mental-health/inequalities/technical-notes.html . Inequality trends for other mental health outcomes (e.g., suicidality, depressive symptomatology, life stress) are shown in the accompanying online data tool at https://health-infobase.canada.ca/mental-health/inequalities/data-tool.html .
5. Discussion and Implications
Although inequities in mental health are determined by a complex interplay of structural and systemic factors, such inequities are all either modifiable or avoidable, and the importance of shifting public health action to address unfair and unjust systemic factors is well recognized Footnote 301 . This report has demonstrated how socioeconomic conditions, sexism, racism, discrimination, colonialism, sense of community belonging and access to health care, affect individual and population mental health , and contribute to mental health inequalities in Canada. Stressful social conditions, and whether people are able to access social support and care, can affect the ability to cope. These social determinants of mental health can be reshaped through intersectoral action. Intersectoral policies and interventions can be co-designed and developed to respond to common challenges and priorities, while advancing mutual goals and benefits to build resilient communities and create equal opportunities and supportive environments for individuals, specific groups, or whole populations. Access to care and individual-level response interventions are an important and necessary aspect of addressing inequalities in mental health, however, such interventions do not address the upstream factors that shape and drive conditions for health, such as the way power is distributed in society and how resources are allocated. Because these upstream or structural factors often happen as a result of decision-making and investments in policies and programs, it is crucial to consider interventions that address mental health and well-being from prevention to treatment, downstream and upstream. Through such approaches, it is possible to improve the conditions in which people live (e.g., socioeconomic conditions, conditions that contribute to discrimination, conditions that foster a sense of community belonging, and conditions under which diverse individuals access and receive mental health treatments and supports), leading to direct and profound impacts on mental health and well-being.
This report combines qualitative evidence and quantitative analysis to provide an overview of the structural drivers of inequalities in mental health. In our analysis, we have referred to systems of power and privilege that maintain and perpetuate inequities in health to show how public health can potentially advocate for, initiate, or facilitate intersectoral collaboration, with the goal of reducing inequities in mental health and well-being. The findings of this work can inform, support, and strengthen the development of research, programs, policies, and plans across multiple sectors to address mental health inequities in Canada.
5 .1 Overview of quantitative trends by theme
The quantitative analyses in this report show population-based inequality trends in high self-rated mental health and life satisfaction across different social dimensions relevant to the four themes identified from the qualitative literature: socioeconomic conditions, racism and discrimination, sense of community belonging, and access, use and quality of health services. Time trends revealed a portrait of how mental health inequalities have changed between 2007 and 2022. Whether inequalities narrowed, persisted, or widened over time varied according to the mental health outcome, the social dimension of inequality, and measurements on the absolute or relative scale.
Between 2007 and 2022, the socioeconomic gradient in mental health was consistent; higher levels of socioeconomic disadvantage (e.g. lower income, food insecurity, housing insecurity, unemployment) were associated with lower life satisfaction. These groups experiencing social disadvantage were also less likely to report high self-rated mental health ( also known as excellent or very good perceived mental health). Income-related disparities in mental health outcomes tended to narrow over time, a trend that largely reflected disproportionate worsening of mental health status among the most economically advantaged groups, especially during the COVID-19 pandemic (see section 4.1.1 for more detail). The associations between other dimensions of material deprivation (food insecurity, housing insecurity, unemployment) and poor mental health persisted or increased over time.
In this time period (2007-2022), mental health inequality trends were analyzed for several population groups that disproportionately experience discrimination in Canada, including racialized, immigrant, and 2SLGBTQI+ populations and Indigenous Peoples. There were significant disparities over time in life satisfaction and high self-rated mental health between both gay/lesbian and bisexual versus heterosexual individuals, racialized immigrants versus White non-immigrants, First Nations living off reserve, Inuit and Métis individuals compared to non-Indigenous individuals, and various racial/ethnicity groups versus White individuals. Between 2007-2010 and 2020-2022, inequalities in high self-rated mental health increased between bisexual and heterosexual individuals. By contrast, inequalities between racialized immigrants versus White non-immigrants in life satisfaction and high self-rated mental health declined, reflecting worsening mental health among White non-immigrants compared to racialized immigrants, especially during the COVID-19 pandemic. Between 2007 and 2022, evidence pointed to persistent inequalities in mental health for First Nations living off reserve, Inuit and Métis people compared to the non-Indigenous population. Analysis of race/ethnicity-related inequalities in self-rated mental health and life satisfaction narrowed for most race/ethnicity groups over time, including and most notably for Black, East/Southeast Asian, South Asian, and Latin Americans, in relation to White individuals. However, some estimates are imprecise due to small sample sizes.
Individuals with a strong sense of community belonging (refer to section 4.1.3) had substantially better mental health and well-being than those with a weaker sense of community belonging. Trend analyses showed consistently worsening mental health among those with a weaker sense of community belonging over time, especially during the COVID-19 pandemic. In addition, First Nations living off-reserve, Inuit and Métis Peoples who reported weak community belonging consistently had lower mean life satisfaction than non-Indigenous individuals who reported weak community belonging. A comparable percentage of long-term and recent immigrants, when compared to non-immigrants, reported having a strong sense of belonging to their local community. However, among males, since 2014-2016, a higher percentage of recent immigrants reported a strong sense of community belonging than non-immigrants. Overall, there was little evidence of immigration-based inequality in strong sense of community belonging. Gay, lesbian, and bisexual individuals consistently reported lower community belonging compared to heterosexual individuals. Among both males and females, the gap was most pronounced between bisexual and heterosexual individuals. Between 2007-2010 and 2020-2022, there was some evidence of an increasing and constant trend in sexual orientation-related inequalities in strong sense of community belonging among females and males, respectively.
Individuals identifying as gay/lesbian/bisexual, immigrants, and racialized respondents reported greater unmet needs for mental health service in 2012 and 2022, compared to heterosexual individuals, non-immigrants, and White individuals, respectively. Additionally, in 2022, females reported a higher rate of unmet need for mental health services than males. Between 2012 and 2022, inequalities in unmet need based on sex/gender and sexual orientation increased, while they decreased based on household income, education level, immigration status, and racialized identity.
5.2 Considerations for Public Health: Findings from Qualitative Synthesis
Our qualitative literature review provided several avenues for intervention to reduce and address inequalities in mental health. These considerations align broadly with the synthesized themes of our review (socioeconomic conditions, racism, xenophobia, homophobia, and other types of discrimination, sense of community belonging, social supports, and cultural connections, and access to, quality of, and use of health care services) and provide suggested future directions for action in public health.
These themes also align closely with public health roles for improving health equity Footnote 302 , which in addition to assessing, reporting, modifying, and orienting interventions, emphasize partnership with other sectors and participation in policy development.
5.2.1 Broadening Understandings of Mental Health, Well-being and Wellness
As discussed in Section 2.1, strictly biomedical understandings of mental health, well-being and wellness limit the potential for more holistic, upstream, strengths-focused, and positive approaches to mental health promotion and care . Through our examination of qualitative studies, we found that the nature and expression of mental distress, or conversely, wellness, was not clearly articulated through language that coincides neatly with standard measures of mental health outcomes in population health surveys. In fact, the categories used to identify problems, measure outcomes, and develop interventions may not fit, for example, newcomers or racialized people, since psychological research has predominantly been based on Western, middle class, educated participants Footnote 303 Footnote 304 . Scholars have noted that many factors, such as “culture, language, ethnicity, and religion influence the causes, manifestations, and course of mental disorders” which can also impact affective symptoms experienced, individual explanations for distress, and how individuals seek help and cope with mental health crises or stressors Footnote 53 .
Our qualitative synthesis reinforces previous bodies of work that outline the need to move beyond considering mental health and wellness exclusively biomedically and psychiatrically, and towards incorporating diverse systems of knowledge, worldviews, experiences, perspectives, communities, and relationships Footnote 305 . This shift can help support more comprehensive and inclusive ways of addressing inequalities in mental health in Canada.
Part of this exercise relates to the role of public health in assessment and reporting Footnote 302 . In order to successfully document the existence and impact of inequities in mental health and develop effective strategies to reduce these inequities, we must pay attention to and bridge multiple ways of knowing and understanding mental health and well-being. An individually focused, biomedically based understanding of mental health and well-being, used often in treatment and care settings, hinders the ability of public health providers and researchers to provide adequate and accurate surveillance of mental health. As some studies have noted Footnote 303 , although inclusion of some biomedical indicators of mental health in surveillance systems is important, different understandings of mental health can impact responses to surveys, and when collected in the context of general health, may be underrepresenting poor mental health and its link to the social determinants Footnote 303 . If mental health is to be understood as a whole-of-society issue, surveillance of mental health outcomes should exist within other surveillance and survey mechanisms—such as through the inclusion of measures related to mental health when collecting data on the labour force, housing, and the environment.
The qualitative research reviewed in this report highlights the limitations of quantitative, population-based research in adequately capturing concepts such as mental health and wellness in a way that meaningfully reflects and measures how it is experienced by diverse population groups in Canada Footnote 53 . In fact, it highlights the important future opportunities for advancing research to measure the wide-ranging nature and depth of experience, and interpretations of meanings of mental health alongside its surveillance. The use of both qualitative and quantitative research, in conjunction with expanded surveillance tools offering respondents a broader conceptualization of mental health, offers opportunities for a more comprehensive understanding of mental health needs and potential public health responses. Additionally, intersectoral collaboration and participatory approaches that can meaningfully link these mental health outcomes with the structural determinants and health are critical.
Acknowledging the distinct worldviews of First Nations, Inuit and Métis peoples as it relates to mental wellness is critical to the discussion of broadening definitions of mental health and well-being. As discussed in section 3.1.2, understanding and acknowledging existing mental wellness frameworks (ex. First Nations Mental Wellness Continuum Framework, Inuit-Specific Mental Wellness Framework and Métis perspectives and worldviews of mental wellness) for Indigenous communities is a crucial and fundamental step when working with Indigenous partners to advance action on mental wellness for these communities. Developing a strong understanding of these frameworks for Indigenous Peoples helps ensure that public health work to improve mental wellness outcomes for Indigenous communities is conducted in a culturally safe manner Footnote 7 Footnote 11 .
5.2.2 Integrating Equity as a Priority in Mental Health Care
Our findings show that individuals identifying as gay/lesbian/bisexual, immigrants, and racialized respondents reported greater unmet needs for mental health service in 2012 and 2022, compared to heterosexual individuals, non-immigrants, and White individuals, respectively. To improve experiences of mental health care among individuals with multiple and intersecting social identities, there is a need to modify and orient interventions to attend to interlocking systems of power and exclusion. Working across disciplines and sectors to mitigate the impact of these systems is a key role of public health. Greater integration of public health systems and mental health care could help address some of the inequalities described in this report in relation to access to mental health care. This could be addressed by supporting the coordination of care, expanding perspectives in clinical practice to include population health, by strengthening health promotion and disease prevention and by facilitating cross-sectoral research, training and policy work in collaboration with the health care sector. International calls expressing the need for greater integration of the health care and public health sectors are not new Footnote 306 . This need has been expressed in seminal international health policy documents, including the 1978 Alma Ata declaration on primary health care and the 1986 Ottawa Charter for Health Promotion Footnote 306 . While this applies to a broad range of health conditions and services, the challenges are particularly relevant for mental health which is often further siloed from physical health services in large part because some mental health services are not financially covered as an under public health insurance plans. This results in differences between how mental health services, physical health services, and upstream public health supports are organized and funded. In addition, the biomedical model for health care means that there are often differences between mental health services and physical health services (as well as public health interventions) in terms of who provides the services and how, including differences in educational requirements and culture Footnote 306 .
Though some roles are more clearly situated in public health and other roles in health care, there are a number of functions for which both public health and health care are responsible, such as planning health care services according to population characteristics and needs, evaluation of the impact of care on patients and communities, advocacy for healthy and equitable communities, and clinical screening and early preventive intervention, among others Footnote 306 . It is at this nexus where the public health and health care sectors can work together and cohesively address intersectional experiences in mental health care. Using an adapted version of Lasker’s models of medicine and public health collaborations Footnote 307 , we describe four categories of functions to advance equity in outcomes for mental health and well-being and associated determinants. We describe specific collaborative actions that both sectors can take, within these functions.
1) Coordinating Care: improving access to mental health services as part of integrated health and mental health care
The studies reviewed as part of this report show that overall, different population groups and individuals with intersecting identities are experiencing challenges in accessing mental health care due to various structural barriers. These include the lack of coordination, communication, and collaboration due to insufficient interaction and integration between health care institutions, health care providers Footnote 278 Footnote 293 and other potential stakeholders (e.g., social work). Other system level difficulties are related to silos of care, the dominance of psychiatric and pharmaceutical treatment for mental health Footnote 285 Footnote 286 , and inadequate training and insufficient numbers of health care providers to address substance use and addictions Footnote 277 . Our report suggests that there is a need and preference for individuals with mental health and substance use issues to receive services in an interdisciplinary and coordinated setting where mental health, physical health and social health are all dealt with and discussed Footnote 278 . Study participants described in positive terms treatment and care they perceived as increasing social connectedness, acceptance, and access to community Footnote 294 . Coordinated care systems that help clients navigate health and mental health services are helpful for communities experiencing health inequities, and a need according to our findings Footnote 306 .
2) Expanding Perspectives: applying a population perspective to clinical practice
Our report includes data and findings on proximal, intermediate, and distal determinants (ex. income, food insecurity, housing, employment) of health that impact and produce inequities in mental health and well-being across the life course for many populations—including Indigenous People, 2SLGBTQI+ individuals, and newcomers. Collaborating with clinicians to share such data and findings in a systematic, comprehensive, and routine way and to identify ways to apply population-level findings to clinical planning is vital. This information can help enhance clinical decision-making by providing an understanding of mental health risks in different communities, supporting outreach programs to help direct communities to programs and treatment, and enhancing practice management (staffing, service provision at various sites) and the development of community mental health and socioeconomic profiles to inform care in communities across Canada Footnote 306 Footnote 309 . Some refer to this as a “learning health system,” the foundation of which is the presence of a data infrastructure used to collect patients’ outcomes Footnote 310 . This data infrastructure typically includes patient-reported experience measures (PREMs) and patient-reported outcome measures (PROMs) that help health care providers tailor their services, enhance patient-centred care, and continuously improve the quality of health care delivery Footnote 311 . These measures become especially useful if they include experiences of discrimination and racism and are disaggregated to delineate intersectional experiences Footnote 312 .
3) Addressing Mental Health Inequalities Through Strengthened Health Promotion and Disease Prevention
Inequalities in mental health and well-being can be reduced through strengthened health promotion and disease prevention. Our findings point to the importance of non-siloed approaches that recognize different life stages, needs, and social determinants, as well as approaches that prioritize partnership with community and civil society. Of particular importance is the need to prioritize culturally responsive and trauma-informed approaches Footnote 184 Footnote 211 , and traditional healing practices that show positive impacts on mental health Footnote 184 . Moreover, approaches that help bridge the gap between health care and community services that address structural and social determinants of health, such as social prescribing interventions, among others, are necessary Footnote 283 . Our findings show associations between mental health inequities and systemic issues such as housing, income, employment, exclusion and alienation, stigma, racism, socioeconomic marginalization, and institutional discrimination. Acting on these system-level determinants of health could potentially help reduce mental health inequities in our communities Footnote 313 .
4) Cross-Sectoral Collaboration between public health and health care
Cross-sectoral collaboration between the public health and health care sectors can help support the translation of research and surveillance related to mental health inequalities into tangible action and interventions. Our findings point to several areas where collaborative training, research, and policy development could help address inequities in mental health and well-being. These areas include social and structural determinants of mental health, culturally sensitive health promotion and health care, homophobia, racial and religious discrimination in different social and institutional settings across the life course, religious and cultural diversity in mental health understandings, intergenerational mental health interventions, and culturally responsive models of mental health care.
5.2.3 Partnering Across Sectors
This report illustrates the importance of considering larger social contexts, conditions, and systems that contribute to inequalities in mental health services in terms of access and availability. Although some actions to tackle mental health inequalities can be addressed by public health, most of the measures that can directly influence the social determinants of health flow from the health system as well as the mandates of other government sectors, community organizations, civil society, and other stakeholders Footnote 314 . Public health partnerships with health system managers and with other ministries and sectors can support more integrated approaches. Addressing upstream factors that shape people’s living conditions increase opportunities and positive outcomes for mental health and well-being.
Canada’s Chief Public Health Officer suggests a coordinated whole-of-society approach that involves partnerships across government, civil society, community, and the private sector to strengthen capacity, coordinate action and respond to public health priorities Footnote 315 . This approach could apply, for example, partnerships with federal ministries that are responsible for income, education, housing, employment or immigration, which could help lead to structural changes that address inequities in mental health and wellness. Additionally, engagement with partners across sectors can maximize investments during times of fiscal austerity. The development of the Canadian Council on Social Determinants of Health by PHAC is one example of engaging with leaders from various sectors to address health equity gaps and the social determinants of health. To date, a number of products have been developed, each of which discuss mental health and wellness. Among these are Roots of Resilience: Overcoming Inequities in Aboriginal Communities and the Pan-Canadian resource on evidence and initiatives to improve the determinants of health for children and their families Footnote 316 .
Engaging with individuals and communities is also necessary in a coordinated whole-of-society approach. Community engagement, particularly with those experiencing disadvantage, mitigates the barriers that more conventional forms of evidence may introduce and helps illuminate needs, strengths, and resiliencies of communities. Such community-focused public health can, therefore, result in improved mental health outcomes, appropriate program development, accessibility, uptake, and fidelity .
Of particular importance is the need to engage with Indigenous partners to advance mental wellness for these communities. Strengthening key partnerships with Federal, Provincial, Territorial, National, and regional organizations was cited as a key element within the distinct wellness plans of First Nations, Inuit and M é tis communities Footnote 7 Footnote 11 . These frameworks emphasize the need for sustained commitment, partnerships, collaboration with major healthcare providers, other service providers, and jurisdictional partners (provincial territorial and federal governments in particular) to ensure the needs of Indigenous Peoples are met. These frameworks emphasize that partnerships must be rooted in guiding principles for First Nations, Inuit and Métis communities, respectively. The First Nations Mental Wellness Continuum Framework, for instance, calls for three guiding principles to direct the establishment of effective partnerships based on mutual respect: Footnote 1 First Nations must be recognized as a key partner, Footnote 2 Partnerships must be complementary where partners have a shared responsibility, and Footnote 3 Partners must know the culture and the reality in which First Nations live, collaborating in ways that reinforce First Nations cultures, traditions, and languages. These frameworks call for regions and communities, working in partnership, to drive changes to the delivery of community based mental wellness programs and services. These frameworks also emphasize the need for national governance structures that privilege “culture as the foundation”, help bridge gaps and promote a systems approach, set out objectives and accountability mechanisms, and monitor and evaluate progress on implementation in partnership with Indigenous communities. They also stipulate the importance of engaging Indigenous communities at the outset as opposed to undertaking consultations once programs or policies have already been developed. Finally, the frameworks underscore the need to define clear roles and responsibilities among Indigenous partners as well as regional, national and federal governments Footnote 7 Footnote 11 .
Our findings point to the need for public health interventions that attend to complex interactions between the determinants of health, such as income, employment, racism, community belonging and access to healthcare, that result in inequities among population groups. Attending to these complex interactions of social determinants requires collaboration across sectors and alongside people with lived experience when developing programs and services to address mental health inequalities and to build resilient communities. Health in All Policies (HiAP) approaches hold promise by advocating for a holistic perspective on health that is systematically integrated into the decision-making processes of all government sectors and departments Footnote 317 . HiAP emphasizes the significance of addressing the underlying causes of health and social issues within policies, across all governmental sectors Footnote 317 . The goal is to achieve synergies that enhance health equity and benefits while minimizing social and health-related harms Footnote 317 . Fundamental to HiAP approaches is the need to attend to the root causes of poor health, such as lack of social protection, and accessibility to services and health care. HiAP is a critical policy lever for addressing inequities in mental health, because many of the drivers for mental health outcomes are beyond the reach of the health sector, as our report has indicated Footnote 317 . Application of HiAP requires an examination of the unintended but potentially foreseeable consequences of policies that are not obviously health related, (for example, Zoning regulations that might impact active transportation and pollution) Footnote 317 .
Collective Impact (CI) offers a structured, cross-sector approach to bringing together diverse stakeholders to tackle complex issues and could be employed by public health and mental health actors seeking to address underlying causes of mental health inequities. CI fundamentally recognizes that mental health is influenced by various social and structural factors. The key principles of CI include partners developing a common agenda, shared measurement system, mutually reinforcing activities, continuous communication, and backbone support organizations Footnote 318 . By bringing together diverse partners such as government agencies, non-profit organizations, health care providers, and community groups, CI allows for a more comprehensive and coordinated approach to addressing the root causes of mental health challenges.
The Quality of Life Framework for Canada is an analytical framework that can help address mental health inequities, particularly at the federal level. This framework looks beyond Gross Domestic Product (GDP) to assess national progress by taking into consideration how federal investments align with 5 holistic domains of Quality of Life (prosperity, health, society, environment, and good governance). The Framework also includes two 2 cross-cutting analytical lenses: Footnote 1 fairness and inclusion, which is intended to inform policy and program development by assessing the distribution of outcomes quality of life indicators for different populations in Canada; and, Footnote 2 sustainability and resilience, intended to promote long-term thinking about quality of life in Canada (taking into account non-economic factors like health housing, environment, and safety) Footnote 319 . This approach to budgeting has a strong potential to shift decision-makers to think more holistically about wellness and create a culture of collaboration across all sectors of government, while also promoting action on the drivers of mental health and well-being.
The findings from this report support a vision for a cohesive intersectoral mental health strategy that is holistic and advances the well-being goals of diverse stakeholders. Implementing such a strategy would facilitate the adoption of holistic approaches to promoting, preventing, and treating mental health issues, beyond conventional mental health care Footnote 320 . This entails collaborating with various sectors to improve the factors influencing mental well-being Footnote 320 . For instance, by enhancing access to education, employment opportunities, housing, and social support systems Footnote 320 . Finland’s National Mental Health Strategy, launched in 2020, provides one example of a collaborative, upstream, national mental health strategy, given its inclusion of multisectoral prevention and treatment activities across public and private sectors as well as non-governmental actors Footnote 321 . In another example, New Zealand’s 2019 Wellbeing Budget, which serves as an example of an upstream policy approach, where government investments and activities – including those for mental health treatment and prevention – were unified under the goal of wellbeing Footnote 322 .
In Canada, a federal multisectoral strategy for mental health might include initiatives from diverse federal departments that address the spectrum of structural, social and environmental determinants that influence mental health and well-being. This strategy could be grounded in the Quality of Life Framework for Canada which recognizes the multiple dimensions that influence overall population well-being, including mental health Footnote 154 . As well, such a strategy could explore whole-of-government processes to assess policies and programs for their impacts on mental well-being and how they can contribute to positive mental health.
5.2.4 Employ universal policies and interventions alongside targeted interventions
In several cases, our findings show a narrowing of inequalities over time driven by worsening rates in the reference group. For instance, in section 4.1.1, our results show how the inequality gap in self-rated mental health by income narrowed over time, primarily reflecting worsening positive mental health status among those with the highest household income, especially during the first year of the COVID-19 pandemic (2020-2022). In section 4.1.2, we show how among both males and females, White non-immigrants showed the greatest reduction in high self-rated mental health over time and racialized immigrants reported the smallest reduction. This translated into notable decreases in high self-rated mental health inequality between racialized immigrants and White non-immigrants, in both absolute and relative terms, for both sexes. When temporal dynamics of inequalities (in this case, narrowing of the divide in positive mental health) is driven by worsening rates in the best-performing or reference group, this is referred to as “levelling down” Footnote 198 . “Levelling down” typically refers to an undesirable change of inequalities (i.e., improvements should be seen by bringing up the level of positive mental health of those who are worse off to that of the best-performing group or “levelling up”).
Alongside this “levelling down” effect seen, our report shows general declines in excellent/very good self-rated mental health across multiple groups (i.e., declines were seen across all income quintiles, in both employed and unemployed groups, across groups experiencing different levels of food insecurity, etc.). These findings suggest that in addition to targeted interventions, there is a need for universal interventions to help address these declines across social strata Footnote 323 . A combination of universal and targeted interventions can help ensure that everyone has the material and social resources to support their mental health Footnote 323 . Interventions may be designed for universal delivery, but implemented at an intensity that is proportionate to need, known as “proportionate universalism” Footnote 324 .
5.2.5 Recognizing and Overcoming Challenges to Data Availability for Health Inequality Monitoring
In Canada, there have been increasing calls for expanding existing population-based surveys, census or administrative databases to address inequalities rooted in systems of power and oppression (e.g., systemic discrimination and racism). The concern is not just overcoming longstanding data gaps by collecting more granular demographic data or data on the structural determinants of health (including climate change and environmental conditions), but ensuring data are relevant and of good quality (e.g., collecting reliable and complete information). It also means systematic data collection, analysis and reporting grounded in cultural responsiveness and accessibility through collaborative engagement with priority populations (i.e., why data are being collected, who data are for, and what is going to happen with them) Footnote 325 Footnote 326 .
Within this context, for the CCHS and other data sources, one way to make improvements is to collect information that challenges the history of discrimination by directly collecting data on racism, race and ethnicity. This includes expanding survey content to ask about experiences of discrimination (overall and across different settings such as healthcare, school, work, interactions with law enforcement). Apart from expanding data collection to topics for which data is currently unavailable, the use of methods for sampling smaller population groups – termed rare populations – is a key consideration. In general, a low number of individuals is a common feature of health inequalities monitoring because data sources are not typically designed with the purpose of having sufficient sample sizes in all population groups. It is, for example, valuable to intentionally include more members of a certain population or community into the sample to produce estimates with adequate levels of precision. This is sometimes referred to as oversampling. When this happens, it may strengthen the capacity to generate new analyses and/or the ability to draw conclusions from the analyses. This is particularly important for intersecting inequalities for which many of the population groups are small or rare types (such as living in low income and in rural areas, belonging to ethnic groups, and being a woman at the same time). Another area for improvement is expanding linkages and harmonizing methods (including questionnaires used) across data sources to provide additional data for health inequality monitoring.
Lastly, as previously mentioned, the CCHS does not capture data for people living on reserves or for people living in northern communities of Quebec that include Inuit Nunangat. To address some of these issues, PHAC has provided financial support to the First Nations Information Governance Centre (FNIGC) to develop a complementary mental wellness report that will be available in 2025. FNIGC’s report will use data from the First Nations Regional Health Survey (RHS), the first and only national First Nations health survey that collects wide-ranging information about First Nations people living on reserve and in northern communities based on western and Traditional understandings of health and well-being. Data from the RHS is collected using an approach built on an inherent respect for data sovereignty in accordance to First Nations principles of OCAP® (Ownership, Control, Access and Possession), which assert that only First Nations have control over data collection processes in their communities, and that they own and control how this information can be stored, interpreted, used, or shared Footnote 325 .
In addition, there is a need for periodic detailed reporting on the magnitude and trends of health inequalities and their determinants to inform potential future policy and program decision-making to more effectively reduce health inequalities, and enable the monitoring of progress in this area, and facilitate collaborative action across jurisdictions.
6. Concluding Remarks
To conclude, our report has explored both qualitative and quantitative evidence, demonstrating the impacts of socioeconomic conditions, racism and discrimination, community belonging and health care access on mental health inequalities. We have summarized how these factors can intersect to produce deep inequalities in mental health and among populations groups. Of note, our findings also indicate that these inequalities have persisted, and in some cases deepened over time.
This report, including the discussion of the broad definitions of mental health and well-being and the use of multiple forms of knowledge to contextualize these understandings, shows new insights into the surveillance and monitoring of mental health inequalities.
Our findings point to important public health actions that can be taken to address these trends in inequalities, including the need to move beyond individualized and pathological conceptualizations of mental health, towards more holistic understandings that attend to structural determinants of health and their impacts, the need to apply population health perspectives in clinical mental health contexts to modify and orient interventions, and the need to partner not only with other government departments but also with community and people to address inequities in mental health.
Acknowledgements
This report was conceptualized and led by a core team within the Health Equity Policy Directorate: Malgorzata Miszkurka, Alexandra Blair, Dolon Chakravartty, Matthew Perks, Nicolas de Guzman Chorny, Shermeen Farooqi, Brittany McKinnon, Julia Mazza, Sai Yi Pan, Rabina Jahan, Radhika Sultania, and Nesrine Bellounar. Technical and content contributions were prepared by Kathleen Dubberly, Mahdis Kamali, Eric Vallières, Natalie Osorio, Ali El-Samra, Kevin Jutras, Ryan De Silva, Ketong Zhou and Tionné Polin.
Gratitude is extended to Health Canada’s librarians for their aid in conducting literature searches for this report. Their expertise and resources enrich the calibre of work produced by the Public Health Agency of Canada.
The report was copy-edited by Joanna Odrowaz, whom we wish to thank for her thorough and thoughtful editorial suggestions.
Steering Committee and Expert Review
The Equity Analysis and Policy Research team within the Strategic Policy Branch of the Public Health Agency of Canada would like to thank the contributions of this report’s Steering Committee, who provided guidance on the scope of the analyses and the interpretation of findings. We would like to thank Steering Committee members, listed in alphabetical order of surname: Paul Bailey (Black Health Alliance), Natalie Gabora-Roth (Public Health Agency of Canada), Dr. Sam Harper (McGill University), Dr. Carla Hilario (University of British Columbia, Okanagan), Dr. Beth Jackson (Public Health Agency of Canada), Helen Kennedy (EGALE Canada), Sarah Kennell (Canadian Mental Health Association), Dr. Laurence Kirmayer (McGill University), Dr. Kwame McKenzie (Wellesley Institute), Dr. Kate Mulligan (University of Toronto), Dr. Cory Neudorf (University of Saskatchewan), Dr. Brenda Restoule (First Peoples Wellness Circle), Dr. Bukola Salami (University of Calgary), Kelly Salmond (Public Health Agency of Canada), Andrea Simpson (Public Health Agency of Canada), and Eduardo Vides (Métis National Council). The conclusions in this report do not necessarily reflect those of the members of the report’s Steering Committee, or their affiliated organizations.
Sections related to First Nations, Inuit, and Métis in this report were co-developed through an iterative collaborative process with Indigenous partners. We would like to humbly thank the following Indigenous organizations and their representatives for their helpful guidance, instruction and input throughout the various stages of the development of this report. We are particularly thankful for the authentic discussions, the knowledge, wisdom, experiences and stories shared with us:
- Assembly of First Nations (represented by the First Peoples Wellness Circle): Dr. Brenda Restoule, Catherine Graham
- Inuit Tapiriit Kanatami: Daniel Afram
- Métis National Council: Ginny Gonneau, Eduardo Vides, Reagan Bartel, Tanya Davoren, Stephen Thomson, Jillian Jones, Shelley Cripps, Emily Paterson, Ryah Heavens, Tanya Pruden, Lori Skjeie, Tegan Brock, Emily Field, Samantha Stewart
This report was also reviewed by several teams internal to the Public Health Agency of Canada, including: the Health Equity Policy Division, Centre for Surveillance and Applied Research and by teams at Health Canada, including: Mental Health And Substance Use Integration Directorate and the Mental Health Division who provided scientific review and advice.
Land acknowledgement
We respectfully acknowledge that the lands on which we live, work, play, and where we developed this report, are the homelands of First Nations, Inuit, and Métis Peoples. Specifically, this report was developed in the following cities:
- In Toronto, also known as Tkaronto, the traditional territory of many nations, including the Mississaugas of the Credit, the Anishnaabeg, the Chippewa, the Haudenosaunee, and the Wendat peoples and is now home to many diverse urban First Nations, Inuit, and Métis Peoples. Toronto is within the lands protected by the Dish with One Spoon Wampum Belt Covenant, an agreement between the Haudenosaunee and Anishinaabe and allied nations to peaceably share and care for the resources around the Great Lakes.
- In Ottawa, also known as Adawe, on the traditional and unceded territory of the Algonquin People, members of the Anishinabek Nation Self-Government Agreement.
- In Montreal, also known as Tiohti:áke, the traditional and unceded territory of the Kanien'kehá:ka. A place which has long served as a site of meeting and exchange amongst many First Nations, including the Kanien'kehá:ka of the Haudenosaunee Confederacy, Huron/Wendat, Abenaki, and Anishinaabeg.
- In Vancouver, on the unceded traditional territories of the xʷməθkʷəy̓əm (Musqueam), Sḵwx̱wú7mesh (Squamish), and səlilwətaɬ (Tsleil-Waututh) Nations.
We recognize that there is much more work ahead to address the harmful impacts of colonialism and racism that continue to generate inequities between Indigenous and non-Indigenous communities.
We respect and affirm the inherent and Treaty Rights of all Indigenous Peoples across this land and uphold the commitments to self-determination and sovereignty made to Indigenous Nations and Peoples.
We acknowledge the historical oppression of lands, cultures and the original Peoples in what we now know as Canada and strive contribute to the healing and decolonizing journey we all share together. We remain strongly committed to working collaboratively to address health inequities across the country.
7. References
- Footnote 1
-
World Health Organization. Health and Well-Being [Internet]. 2023 [cited 2023 Sep 22]. Available from: https://www.who.int/data/gho/data/major-themes/health-and-well-being
- Footnote 2
-
World Health Organization. Social determinants of health [Internet]. 2021 [cited 2023 Aug 29]. Available from: https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1
- Footnote 3
-
World Health Organization. Rio Political Declaration on Social Determinants of Health. In: World Conference on Social Determinants of Health [Internet]. Rio de Janeiro, Brazil: World Health Organization; 2011. Available from: https://www.who.int/publications/m/item/rio-political-declaration-on-social-determinants-of-health
- Footnote 4
-
Government of Canada. Federal Anti-Racism Secretariat [Internet]. 2021 [cited 2023 Sep 6]. Available from: https://www.canada.ca/en/canadian-heritage/campaigns/federal-anti-racism-secretariat.html
- Footnote 5
-
Government of Canada. Federal 2SLGBTQI+ Action Plan: Building our future, with pride [Internet]. 2023 [cited 2024 Jan 12]. Available from: https://women-gender-equality.canada.ca/en/free-to-be-me/federal-2slgbtqi-plus-action-plan.html
- Footnote 6
-
Harvey I. Rose’s Strategy of Preventative Medicine. Public Health. 2009;123(10).
- Footnote 7
-
Alianait Inuit-specific Mental Wellness Task Group. Alianait Inuit Mental Wellness: Action Plan [Internet]. Inuit Tapiriit Kanatami; 2007. Available from: http://docplayer.net/18015067-Alianait-inuit-mental-wellness-action-plan-prepared-by-alianait-inuit-specific-mental-wellness-task-group.html
- Footnote 8
-
Dumont J. First Nations Regional Longitudinal Health Survey (RHS) Cultural Framework [Internet]. First Nations Information Governance Centre (FNIGC); 2005. Available from: https://web.archive.org/web/20200919111946/http://fnigc.ca/sites/default/files/ENpdf/RHS_General/developing-a-cultural-framework.pdf
- Footnote 9
-
National Aboriginal Health Organization. In The Words of Our Ancestors: Métis Health and Healing. 2008.
- Footnote 10
-
British Columbia Office of the Provincial Health Officer, Métis Nation British Columbia. Taanishi Kiiya? Miiyayow Métis Saantii Pi Miyooayaan Didaan BC: Métis Public Health Surveillance Program—Baseline Report, 2021. 2021.
- Footnote 11
-
Health Canada. First Nations Mental Wellness Continuum Framework. Ottawa, ON; 2015.
- Footnote 12
-
Solar O, Irwin A. A Conceptual Framework for Action on the Social Determinants of Health [Internet]. 2010. Available from: https://apps.who.int/iris/bitstream/handle/10665/44489/9789241500852_eng.pdf?sequence=1&isAllowed=y
- Footnote 13
-
Public Health Agency of Canada. Key health inequalities in Canada: A national portrait. Public Health Agency of Canada Ottawa, Ontario; 2018.
- Footnote 14
-
Public Health Agency of Canada (PHAC). How to integrate intersectionality theory in quantitative health equity analysis? A rapid review and checklist of promising practices [Internet]. 2022. Available from: https://www.canada.ca/en/public-health/services/publications/science-research-data/how-integrate-intersectionality-theory-quantitative-health-equity-analysis.html#a1
- Footnote 15
-
Lim KL, Jacobs P, Ohinmaa A, Schopflocher D, Dewa CS. A new population-based measure of the economic burden of mental illness in Canada. Chronic Dis Can [Internet]. 2008;28(3). Available from: https://www.canada.ca/content/dam/phac-aspc/migration/phac-aspc/publicat/hpcdp-pspmc/28-3/pdf/cdic28-3-2eng.pdf
- Footnote 16
-
CAMH. Mental Health in Canada: Covid-19 and Beyond [Internet]. 2020. Available from: https://www.camh.ca/-/media/files/pdfs---public-policy-submissions/covid-and-mh-policy-paper-pdf.pdf
- Footnote 17
-
World Health Organization. Constitution of the World Health Organization. Basic Documents. Geneva; 1946.
- Footnote 18
-
Whitehead M. The concepts and principles of equity and health. Vol. 22, International Journal of Health Services. 1992.
- Footnote 19
-
Ruger JP. Health and Social Justice. Health and Social Justice. 2010.
- Footnote 20
-
Schillinger D, Barton LR, Karter AJ, Wang F, Adler N. Does literacy mediate the relationship between education and health outcomes? A study of a low-income population with diabetes. Public Health Rep. 2006;121(3).
- Footnote 21
-
Shim R, Koplan C, Langheim FJP, Manseau MW, Powers RA, Compton MT. The social determinants of mental health: An overview and call to action. Vol. 44, Psychiatric Annals. 2014.
- Footnote 22
-
Public Health Agency of Canada. Social determinants of health and health inequalities [Internet]. 2022 [cited 2023 May 25]. Available from: https://www.canada.ca/en/public-health/services/health-promotion/population-health/what-determines-health.html
- Footnote 23
-
Solar O, Irwin A, World Health Organization. A conceptual framework for action on the social determinants of health. WHO Document Production Services; 2010.
- Footnote 24
-
Public Health Agency of Canada, Tam T. Addressing stigma: Towards a more inclusive health system. 2019.
- Footnote 25
-
Labonté R, Stuckler D. The rise of neoliberalism: How bad economics imperils health and what to do about it. J Epidemiol Community Health. 2016;70(3).
- Footnote 26
-
Abdillahi I, Shaw A. Public Health Agency of Canada. 2020. p. 1–14 Social determinants and inequities in health for Black Canadians: A Snapshot.
- Footnote 27
-
Canadian Mental Health Association. 2022. Social Determinants of Health.
- Footnote 28
-
Mikkonen J, Raphael D. The Canadian Facts. 2010. Social Determinants of Health: The Canadian Facts.
- Footnote 29
-
Compton MT, Shim RS. Why Employers Must Focus on the Social Determinants of Mental Health. Vol. 34, American journal of health promotion. United States; 2020. p. 215–9.
- Footnote 30
-
Galderisi S, Heinz A, Kastrup M, Beezhold J, Sartorius N. Toward a new definition of mental health. World Psychiatry. 2015;14(2):231.
- Footnote 31
-
Manwell LA, Barbic SP, Roberts K, Durisko Z, Lee C, Ware E, et al. What is mental health? Evidence towards a new definition from a mixed methods multidisciplinary international survey. BMJ Open. 2015;5(6).
- Footnote 32
-
Hankivsky O. Intersectionality 101 [Internet]. 2014. Available from: https://bccampus.ca/wp-content/uploads/2020/07/Hankivsky-Intersectionality101-2014.pdf
- Footnote 33
-
Collins AB, Boyd J, Cooper HLF, McNeil R. The intersectional risk environment of people who use drugs. Soc Sci Med. 2019 Aug 1;234.
- Footnote 34
-
National Collaborating Centre for Determinants of Health. Glossary of essential health equity terms [Internet]. Antigonish, Nova Scotia; 2022. Available from: https://nccdh.ca/learn/glossary
- Footnote 35
-
Public Health Agency of Canada (PHAC). Positive Mental Health Surveillance Indicator Framework [Internet]. 2023 [cited 2023 Sep 6]. Available from: https://health-infobase.canada.ca/positive-mental-health/
- Footnote 36
-
World Health Organization. Health Promotion [Internet]. 2012 [cited 2024 Apr 3]. Available from: https://www.who.int/teams/health-promotion/enhanced-wellbeing/first-global-conference
- Footnote 37
-
Deacon BJ. The biomedical model of mental disorder: A critical analysis of its validity, utility, and effects on psychotherapy research. Vol. 33, Clinical Psychology Review. 2013.
- Footnote 38
-
Golden TL, Wendel ML. Public Health’s Next Step in Advancing Equity: Re-evaluating Epistemological Assumptions to Move Social Determinants From Theory to Practice. Front Public Heal. 2020;8.
- Footnote 39
-
Parker G, Tavella G, Macqueen G, Berk M, Grunze H, Deckersbach T, et al. Revising Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, criteria for the bipolar disorders: Phase I of the AREDOC project. Aust N Z J Psychiatry. 2018;52(12).
- Footnote 40
-
Harrison JE, Weber S, Jakob R, Chute CG. ICD-11: an international classification of diseases for the twenty-first century. Vol. 21, BMC Medical Informatics and Decision Making. 2021.
- Footnote 41
-
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DMS-5). 5th ed. Vol. 21. American Psychiatric Pub; 2013.
- Footnote 42
-
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Fifth Edit. 2013.
- Footnote 43
-
Manderscheid R, Ryff C, … EFP chronic, 2010 U. Peer reviewed: evolving definitions of mental illness and wellness. ncbi.nlm.nih.gov. 2010.
- Footnote 44
-
Keyes CLM. Promoting and protecting mental health as flourishing: A complementary strategy for improving national mental health. Am Psychol. 2007;62(2):95–108.
- Footnote 45
-
Public Health Agency of Canada (PHAC). Mental Health Continuum Model (MHCM) [Internet]. 2023 [cited 2023 Sep 6]. Available from: https://www.canada.ca/en/department-national-defence/corporate/reports-publications/health/r2mr-aide-memoire/mental-health-continuum-model.html
- Footnote 46
-
Orpana H, Vachon J, Dykxhoorn J, Jayaraman G. Measuring positive mental health in Canada: Construct validation of the mental health continuum-short form. Heal Promot Chronic Dis Prev Canada. 2017;37(4).
- Footnote 47
-
Iasiello M, van Agteren J, Cochrane EM. Mental Health and/or Mental Illness: A Scoping Review of the Evidence and Implications of the Dual-Continua Model of Mental Health. Evid Base. 2020;2020(1).
- Footnote 48
-
Government of Canada. Canadian Chronic Disease Indicators (CCDI) [Internet]. 2023 [cited 2023 Sep 26]. Available from: https://health-infobase.canada.ca/ccdi/data-tool/
- Footnote 49
-
Statistics Canada. Table 13-10-0096-18 Mood disorders, by age group [Internet]. 2023 [cited 2023 Sep 26]. Available from: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310009618
- Footnote 50
-
Orpana HM, Vachon J, Pearson C, Elliott K, Smith M, Branchard B. Correlates of well-being among Canadians with mood and/or anxiety disorders. Heal Promot Chronic Dis Prev Canada Res Policy Pract [Internet]. 2016;36(12). Available from: https://www.canada.ca/en/public-health/services/reports-publications/health-promotion-chronic-disease-prevention-canada-research-policy-practice/vol-36-no-12-2016/correlates-well-being-among-canadians-with-mood-anxiety-disorders.html
- Footnote 51
-
Public Health Agency of Canada (PHAC). Mental Health Promotion [Internet]. 2014 [cited 2023 Sep 6]. Available from: https://www.canada.ca/en/public-health/services/health-promotion/mental-health/mental-health-promotion.html
- Footnote 52
-
Orpana H, Vachon J, Dykxhoorn J, McRae L, Jayaraman G. Monitoring positive mental health and its determinants in Canada: the development of the Positive Mental Health Surveillance Indicator Framework. Heal Promot Chronic Dis Prev Canada [Internet]. 2016;36(1). Available from: https://www.canada.ca/en/public-health/services/reports-publications/health-promotion-chronic-disease-prevention-canada-research-policy-practice/vol-36-no-1-2016/monitoring-positive-mental-health-its-determinants-canada-development-positive-mental-health-
- Footnote 53
-
Kirmayer LJ. Cultural competence and evidence-based practice in mental health: Epistemic communities and the politics of pluralism. Vol. 75, Social Science and Medicine. 2012.
- Footnote 54
-
Heller JC, Fleming PJ, Petteway RJ, Givens M, Porter KMP. Power Up: A Call for Public Health to Recognize, Analyze, and Shift the Balance in Power Relations to Advance Health and Racial Equity. Am J Public Health. 2023;113(10).
- Footnote 55
-
Tagalik S. Inuit Qaujimajatuqangit: The role of Indigenous knowledge in supporting wellness in Inuit communities in Nunavut. 2011;
- Footnote 56
-
Macdougall B. Land, family and identity: contextualizing Metis health and well-being. National Collaborating Centre for Aboriginal Health Prince George; 2017.
- Footnote 57
-
Gaudry A, Corntassel J. Insurgent education and indigenous-centred research: Opening new pathways to community resurgence. In: Learning and Teaching Community-Based Research: Linking Pedagogy to Practice. Toronto, ON: University of Toronto Press; 2014. p. 167–85.
- Footnote 58
-
Fijal D, Beagan BL. Indigenous perspectives on health: Integration with a Canadian model of practice. Can J Occup Ther. 2019;86(3).
- Footnote 59
-
Halseth R, Murdock L. Supporting Indigenous self-determination in health: Lessons learned from a review of best practices in health governance in Canada and internationally. 2020;
- Footnote 60
-
Thunderbird Partnership Foundation. The Indigenous Wellness Framework Reference Guide [Internet]. 2020. Available from: https://thunderbirdpf.org/wp-content/uploads/2022/03/indigenous_wellness_framework_reference_guide.pdf
- Footnote 61
-
Inuit Tapiriit Kanatami. National Inuit Suicide Prevention Strategy [Internet]. 2016 [cited 2023 Sep 8]. Available from: https://www.itk.ca/national-inuit-suicide-prevention-strategy/
- Footnote 62
-
Kinnon D. Engaging Inuit Men and Boys in Ending Violence Against Women and Girls: A gender-based analysis [Internet]. Ottawa, ON; 2014. Available from: https://pauktuutit.ca/project/engaging-inuit-men-boys-ending-violence-women-girls-gender-based-analysis/
- Footnote 63
-
Métis National Council. Métis Vision for Health [Internet]. 2022. Available from: https://www.metisnation.ca/uploads/documents/3-1)Métis Vision for Health-July 12 update.pdf
- Footnote 64
-
Graham C, Davoren T. Sharing their Stories: Narratives of young Métis parents and Elders about parenting. National Collaborating Centre for Aboriginal Health Prince George, BC; 2015.
- Footnote 65
-
Les Femmes Michif Otipemisiwak = Women of the Métis Nation. Métis Perspectives of Missing and Murdered Indigenous Women, Girls and LGBTQ2S+ People [Internet]. Les Femmes Michif Otipemisiwak = Women of the Métis Nation; 2019. Available from: https://web.archive.org/web/20200213194800/https://en2.metiswomen.org/wp-content/uploads/2019/11/LFMO-MMIWG-Report.pdf
- Footnote 66
-
Tourand J, Stewart D, Peled M, Poon C, Smith A. Ta Saantii: A Profile of Métis Youth Health in BC. 2016.
- Footnote 67
-
Collins PH. Black feminist thought in the matrix of domination. Black Fem thought Knowledge, consciousness, Polit Empower. 1990;138(1990):221–38.
- Footnote 68
-
Collins PH. Gender, black feminism, and black political economy. Ann Am Acad Pol Soc Sci. 2000;568(1):41–53.
- Footnote 69
-
Hill Collins P, Bilge S. Intersectionality. Cambridge, UK: Polity Press; 2016.
- Footnote 70
-
Haines-Saah R, Hilario CT, Jenkins EK, Ng CKY, Johnson JL. Understanding adolescent narratives about “bullying” through an intersectional lens: Implications for youth mental health interventions. Youth Soc [Internet]. 2018;50(5):636–58. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=psyc15&NEWS=N&AN=2018-27319-004
- Footnote 71
-
Crenshaw K. Demarginalizing the intersection of race and sex: A black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. u Chi Leg f. 1989;139.
- Footnote 72
-
Hill Collins P, Bilge SS. Intersectionality. Key Concepts Series. Cambridge. Cambridge, UK: Polity Press; 2016.
- Footnote 73
-
Bowleg L. The Problem With the Phrase Women and Minorities: Intersectionality—an Important Theoretical Framework for Public Health. Am J Public Health. 2012;102(7):1267–73.
- Footnote 74
-
Ford CL, Airhihenbuwa CO. Critical race theory, race equity, and public health: Toward antiracism praxis. Vol. 100, American Journal of Public Health. 2010.
- Footnote 75
-
Eakin JM. Educating Critical Qualitative Health Researchers in the Land of the Randomized Controlled Trial. Qual Inq. 2016;22(2).
- Footnote 76
-
Mays N, Pope C. Quality in qualitative research. In: Qualitative Research in Health Care. 2019.
- Footnote 77
-
Dobbins M. Rapid Review Guidebook: Steps for conducting a rapid review. Natl Collab Cent Method Tools. 2017;
- Footnote 78
-
Alegría M, NeMoyer A, Falgàs Bagué I, Wang Y, Alvarez K. Social Determinants of Mental Health: Where We Are and Where We Need to Go. Vol. 20, Current Psychiatry Reports. 2018.
- Footnote 79
-
Allen J, Balfour R, Bell R, Marmot M. Social determinants of mental health. Int Rev Psychiatry. 2014;26(4):392–407.
- Footnote 80
-
Silva M, Loureiro A, Cardoso G. Social determinants of mental health: A review of the evidence. Vol. 30, European Journal of Psychiatry. 2016.
- Footnote 81
-
Compton MT, Shim RS. The social determinants of mental health clinical synthesis. Focus (Madison). 2015;13(4).
- Footnote 82
-
Centre FNIG. Strengths-Based Approaches to Indigenous Research and the Development of Well-Being Indicators [Internet]. Ottawa, ON; 2020. Available from: https://fnigc.ca/wp-content/uploads/2021/05/FNIGC-Research-Series-SBA_v04.pdf
- Footnote 83
-
Government of Canada. Measuring What Matters: Toward a Quality of Life Strategy for Canada [Internet]. Ottawa, ON; 2021. Available from: https://www.canada.ca/en/department-finance/services/publications/measuring-what-matters-toward-quality-life-strategy-canada.html
- Footnote 84
-
OECD. Better Life Initiative: Measuring Well-Being and Progress [Internet]. 2020. Available from: https://www.oecd.org/wise/better-life-initiative.htm#:~:text=The OECD Better Life Initiative and the work,be done to achieve greater progress for all.
- Footnote 85
-
Public Health Agency of Canada (PHAC). Key Health Inequalities in Canada: A National Portrait [Internet]. Ottawa, ON; 2018. Available from: https://www.canada.ca/content/dam/phac-aspc/documents/services/publications/science-research/key-health-inequalities-canada-national-portrait-executive-summary/key_health_inequalities_full_report-eng.pdf
- Footnote 86
-
Public Health Agency of Canada (PHAC). Canadian Chronic Disease Surveillance System (CCDSS) [Internet]. 2023 [cited 2023 Sep 6]. Available from: https://health-infobase.canada.ca/ccdss/data-tool/
- Footnote 87
-
Public Health Agency of Canada (PHAC). How healthy are people in Canada? An indicators dashbaord. [Internet]. 2023 [cited 2023 Oct 6]. Available from: https://health-infobase.canada.ca/health-of-people-in-Canada-dashboard/
- Footnote 88
-
Public Health Agency of Canada (PHAC). Pan-Canadian Health Inequalities Data Tool. A joint initiative of the Public Health Agency of Canada, the Pan-Canadian Public Health Network, Statistics Canada and the Canadian Institute for Health Information [Internet]. [cited 2023 Sep 6]. Available from: https://health-infobase.canada.ca/health-inequalities/data-tool/index
- Footnote 89
-
Goel V, Rosella LC, Fu L, Alberga A. The relationship between life satisfaction and healthcare utilization: A longitudinal study. Am J Prev Med. 2018;55(2).
- Footnote 90
-
Rosella LC, Fu L, Buajitti E, Goel V. Death and Chronic Disease Risk Associated with Poor Life Satisfaction: A Population-Based Cohort Study. Am J Epidemiol. 2019;188(2).
- Footnote 91
-
Findlay L, Arim R. Canadians report lower self-perceived mental health during the COVID-19 pandemic. Statistics Canada. 2020.
- Footnote 92
-
Helliwell JF, Schellenberg G, Fonberg J. Life Satisfaction in Canada Before and During the COVID-19 Pandemic. Anal Stud Branch Res Pap Ser. 2020;(11).
- Footnote 93
-
Aknin LB, De Neve JE, Dunn EW, Fancourt DE, Goldberg E, Helliwell JF, et al. Mental Health During the First Year of the COVID-19 Pandemic: A Review and Recommendations for Moving Forward. Perspect Psychol Sci. 2022;17(4).
- Footnote 94
-
OECD. OECD Better Life Index: Canada [Internet]. 2023 [cited 2023 Sep 26]. Available from: https://www.oecdbetterlifeindex.org/countries/canada/
- Footnote 95
-
OECD. How’s Life? 2020: Measuring well-being. OECD Publishing. 2020.
- Footnote 96
-
Lund C, Brooke-Sumner C, Baingana F, Baron EC, Breuer E, Chandra P, et al. Social determinants of mental disorders and the Sustainable Development Goals: a systematic review of reviews. The Lancet Psychiatry. 2018 Apr 1;5(4):357–69.
- Footnote 97
-
Ribeiro WS, Bauer A, Andrade MCR, York-Smith M, Pan PM, Pingani L, et al. Income inequality and mental illness-related morbidity and resilience: a systematic review and meta-analysis. The Lancet Psychiatry. 2017 Jul 1;4(7):554–62.
- Footnote 98
-
Vanzella-Yang A, Veenstra G. Social mobility and mental health in Canada. Can J Public Heal [Internet]. 2023; Available from: https://pubmed.ncbi.nlm.nih.gov/37801229/
- Footnote 99
-
Levesque AR, MacDonald S, Berg SA, Reka R. Assessing the Impact of Changes in Household Socioeconomic Status on the Health of Children and Adolescents: A Systematic Review. Vol. 6, Adolescent Research Review. 2021.
- Footnote 100
-
Ridley M, Rao G, Schilbach F, Patel V. Poverty, depression, and anxiety: Causal evidence and mechanisms. Science (80- ) [Internet]. 2020 Dec 11 [cited 2023 Aug 23];370(6522). Available from: https://www.science.org/doi/10.1126/science.aay0214
- Footnote 101
-
Thomson RM, Igelström E, Purba AK, Shimonovich M, Thomson H, McCartney G, et al. How do income changes impact on mental health and wellbeing for working-age adults? A systematic review and meta-analysis. Lancet Public Heal. 2022 Jun 1;7(6):e515–28.
- Footnote 102
-
Patel V, Burns JK, Dhingra M, Tarver L, Kohrt BA, Lund C. Income inequality and depression: a systematic review and meta-analysis of the association and a scoping review of mechanisms. World Psychiatry. 2018;17(1):76–89.
- Footnote 103
-
Pickett KE, Wilkinson RG. Inequality: an underacknowledged source of mental illness and distress. Br J Psychiatry. 2018;197(6):426–8.
- Footnote 104
-
Tarasuk V, Li T, Fafard St-Germain A. Household Food Insecurity in Canada, 2021 [Internet]. Toronto; 2022. Available from: https://proof.utotoronto.ca/
- Footnote 105
-
Shafiee M, Vatanparast H, Janzen B, Serahati S, Keshavarz P, Jandaghi P, et al. Household food insecurity is associated with depressive symptoms in the Canadian adult population. J Affect Disord. 2021 Jan 15;279:563–71.
- Footnote 106
-
Men F, Elgar FJ, Tarasuk V. Food insecurity is associated with mental health problems among Canadian youth. J Epidemiol Community Heal [Internet]. 2021 Aug 1 [cited 2023 Aug 23];75(8):741–8. Available from: https://jech.bmj.com/content/75/8/741
- Footnote 107
-
Polsky JY, Gilmour H. Food insecurity and mental health during the COVID-19 pandemic [Internet]. 2020 Dec [cited 2023 Aug 23]. Available from: https://www.doi.org/10.25318/82-003-x202001200001-eng
- Footnote 108
-
Commission CHR. Housing is a human right [Internet]. 2019. Available from: https://www.chrc-ccdp.gc.ca/en/node/717
- Footnote 109
-
Statistics Canada. Core housing need in Canada [Internet]. 2022 [cited 2023 Aug 24]. Available from: https://www150.statcan.gc.ca/n1/pub/11-627-m/11-627-m2022056-eng.htm
- Footnote 110
-
Singh A, Daniel L, Baker E, Bentley R. Housing Disadvantage and Poor Mental Health: A Systematic Review. Am J Prev Med. 2019 Aug 1;57(2):262–72.
- Footnote 111
-
S.A. K, G. V, T. K, D. B, D. H, I. M, et al. The role of gender in housing for individuals with severe mental illness: A qualitative study of the Canadian service context. BMJ Open [Internet]. 2013;3(6):e002914. Available from: http://bmjopen.bmj.com/content/3/6/e002914.full.pdf+html
- Footnote 112
-
Statistics Canada. The Daily. 2021 [cited 2024 Feb 6]. One in five Canadians with mental health-related disabilities lives in core housing need. Available from: https://www150.statcan.gc.ca/n1/daily-quotidien/210128/dq210128d-eng.htm
- Footnote 113
-
Strobel S, Burcul I, Dai JH, Ma Z, Jamani S, Hossain R. Characterizing people experiencing homelessness and trends in homelessness using population-level emergency department visit data in Ontario, Canada. Ottawa; 2021 Jan.
- Footnote 114
-
Government of Canada. Everyone Counts 2020-2022: Preliminary Highlights Report. 2023.
- Footnote 115
-
Palepu A, Hubley AM, Russell LB, Gadermann AM, Chinni M. Quality of life themes in Canadian adults and street youth who are homeless or hard-to-house: A multi-site focus group study. Health Qual Life Outcomes. 2012;10.
- Footnote 116
-
Monari E, Booth R, Harerimana B, Forchuk C. The Experiences of Migration among Homeless Male and Female Psychiatric Survivors. Issues Ment Health Nurs [Internet]. 2020;41(6):467–75. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med18&NEWS=N&AN=32356675
- Footnote 117
-
Statistics Canada. Housing conditions among First Nations people, Métis and Inuit in Canada from the 2021 Census [Internet]. 2022. Available from: https://www12.statcan.gc.ca/census-recensement/2021/as-sa/98-200-X/2021007/98-200-X2021007-eng.cfm
- Footnote 118
-
Statistics Canada. Aboriginal Peoples Survey, 2012 - Social determinants of health for the off-reserve First Nations population, 15 years of age and older, 2012 [Internet]. 2016. Available from: https://www150.statcan.gc.ca/n1/pub/89-653-x/89-653-x2016010-eng.htm
- Footnote 119
-
Brandon J, Peters E. Moving to the City: Housing and Aboriginal Migration to Winnipeg [Internet]. Winnipeg; 2014. Available from: https://policyalternatives.ca/sites/default/files/uploads/publications/Manitoba Office/2014/12/Aboriginal_Migration.pdf
- Footnote 120
-
Atkey J, Chau L, Falvo N, Flynn A, Gurstein P, Jones C, et al. The Municipal Role in Housing. 2022.
- Footnote 121
-
Mason KE, Baker E, Blakely T, Bentley RJ. Housing affordability and mental health: Does the relationship differ for renters and home purchasers? Soc Sci Med [Internet]. 2013;94:91–7. Available from: https://www.sciencedirect.com/science/article/pii/S0277953613003547?via%3Dihub
- Footnote 122
-
Giannoni M, Grignon M. Food insecurity, home ownership and income-related equity in dental care use and access: the case of Canada. BMC Public Health. 2022;22(1).
- Footnote 123
-
Dhunna S, Tarasuk V. Black–white racial disparities in household food insecurity from 2005 to 2014, Canada. Can J Public Heal. 2021;112(5).
- Footnote 124
-
Van Der Noordt M, Ijzelenberg H, Droomers M, Proper KI. Health effects of employment: a systematic review of prospective studies. 2014 [cited 2023 Aug 24]; Available from: http://dx.doi.org/10.1136/
- Footnote 125
-
Amiri S. Unemployment associated with major depression disorder and depressive symptoms: a systematic review and meta-analysis. https://doi.org/101080/1080354820211954793. 2021;28(4):2080–92.
- Footnote 126
-
Kim TJ, von dem Knesebeck O. Perceived job insecurity, unemployment and depressive symptoms: a systematic review and meta-analysis of prospective observational studies. Int Arch Occup Environ Health [Internet]. 2016 May 1 [cited 2023 Aug 24];89(4):561–73. Available from: https://link.springer.com/article/10.1007/s00420-015-1107-1
- Footnote 127
-
Norström F, Virtanen P, Hammarström A, Gustafsson PE, Janlert U. How does unemployment affect self-Assessed health? A systematic review focusing on subgroup effects. BMC Public Health [Internet]. 2014 Dec 22 [cited 2023 Aug 24];14(1):1–13. Available from: https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-14-1310
- Footnote 128
-
Harvey SB, Modini M, Joyce S, Milligan-Saville J, Tan L, Mykletun A, et al. Can work make you mentally ill? A systemic meta-review of work-related risk factors for common mental health problems. Occup Environ Med [Internet]. 17AD;74:301–10. Available from: https://oem.bmj.com/content/oemed/74/4/301.full.pdf
- Footnote 129
-
CMHA. Ending the Healthcare Disparity in Canada. 2018.
- Footnote 130
-
Wayne L, Michelynn L. Precarious Employment and Social Outcomes. Just Labour. 2014;
- Footnote 131
-
National Collaborating Centre for Indigenous Health. Employment as a social determinant of First Nations, Inuit, and Métis health [Internet]. 2017. Available from: https://www.ccnsa-nccah.ca/docs/determinants/FS-Employment-SDOH-2017-EN.pdf
- Footnote 132
-
George U, Thomson MS, Chaze F, Guruge S. Immigrant Mental Health, A Public Health Issue: Looking Back and Moving Forward. Int J Environ Res Public Health [Internet]. 2015;12(10):13624–48. Available from: https://www.mdpi.com/1660-4601/12/10/13624
- Footnote 133
-
Premji S, Shakya Y. Pathways between under/unemployment and health among racialized immigrant women in Toronto. Ethn Heal. 2017;22(1).
- Footnote 134
-
Hilario CT, Oliffe JL, Wong JP, Browne AJ, Johnson JL. “Just as Canadian as Anyone Else”? Experiences of Second-Class Citizenship and the Mental Health of Young Immigrant and Refugee Men in Canada. Am J Mens Health [Internet]. 2018;12(2):210–20. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med15&NEWS=N&AN=29183223
- Footnote 135
-
Premji S. “It’s Totally Destroyed Our Life”: Exploring the Pathways and Mechanisms Between Precarious Employment and Health and Well-being Among Immigrant Men and Women in Toronto. Int J Heal Serv. 2018;48(1).
- Footnote 136
-
Creese G, Wiebe B. “Survival Employment”: Gender and Deskilling among African Immigrants in Canada. Int Migr [Internet]. 2012;50(5):56–76. Available from: https://onlinelibrary.wiley.com/doi/full/10.1111/j.1468-2435.2009.00531.x
- Footnote 137
-
Grant PR, Nadin S. The Credentialing Problems of Foreign Trained Personnel from Asia and Africa Intending to Make their Home in Canada: A Social Psychological Perspective. J Int Migr Integr [Internet]. 2007;8:141–62. Available from: https://link.springer.com/article/10.1007/s12134-007-0011-2
- Footnote 138
-
Patel A, Dean J, Edge S, Wilson K, Ghassemi E. Double Burden of Rural Migration in Canada? Considering the Social Determinants of Health Related to Immigrant Settlement Outside the Cosmopolis. Int J Environ Res Public Heal [Internet]. 2019;16(5):678. Available from: https://www.mdpi.com/1660-4601/16/5/678
- Footnote 139
-
Ramjattan VA. Racializing the problem of and solution to foreign accent in business. Appl Linguist Rev [Internet]. 2019;13(4):527–44. Available from: https://www.degruyter.com/document/doi/10.1515/applirev-2019-0058/html
- Footnote 140
-
Houle R, Yssaad L. Recognition of newcomers’ foreign credentials and work experience. Perspect Labour Income. 2010;11(9).
- Footnote 141
-
Guo Y. Racializing immigrant professionals in an employment preparation ESL program. Cult Pedagog Inq [Internet]. 2009;1(2). Available from: https://journals.library.ualberta.ca/cpi/index.php/cpi/article/view/7119
- Footnote 142
-
Government of Canada. National Occupation Classification [Internet]. 2021. Available from: https://noc.esdc.gc.ca/Versions/VersionsWelcome
- Footnote 143
-
Statistics Canada. The impact of COVID-19 on the Canadian labour market [Internet]. Ottawa, ON; 2020. Available from: https://www150.statcan.gc.ca/n1/pub/11-627-m/11-627-m2020028-eng.htm
- Footnote 144
-
Ghabrial MA, Scheim AI, Chih C, Santos H, Adams NJ, Bauer GR. Change in Finances, Peer Access, and Mental Health Among Trans and Nonbinary People During the COVID-19 Pandemic. LGBT Heal. 2023;
- Footnote 145
-
Egale. “Not sure how much longer I can hold on”: The pandemic’s impacts on housing, income, food security, and mental health among 2SLGBTQI people [Internet]. 2023. Available from: https://egale.ca/wp-content/uploads/2023/09/QMH-Data-Brief-1.pdf
- Footnote 146
-
Haw C, Hawton K, Gunnell D, Platt S. Economic recession and suicidal behaviour: Possible mechanisms and ameliorating factors. Int J Soc Psychiatry [Internet]. 2014;61(1). Available from: https://journals.sagepub.com/doi/10.1177/0020764014536545
- Footnote 147
-
Volkos P, Symvoulakis E. Impact of financial crisis on mental health: A literature review ‘puzzling’ findings from several countries. 2International J Soc Psychiatry [Internet]. 2021;67(7). Available from: https://journals.sagepub.com/doi/abs/10.1177/00207640211011205?journalCode=ispa
- Footnote 148
-
Government of Canada. Inequalities in the mental health of adults before and during the COVID-19 pandemic: summary [Internet]. Ottawa, ON; 2022. Available from: https://health-infobase.canada.ca/covid-19/mental-health-inequalities/summary.html
- Footnote 149
-
Jenkins EK, McAuliffe C, Hirani S, Richardson C, Thomson KC, McGuinness L, et al. A portrait of the early and differential mental health impacts of the COVID-19 pandemic in Canada: Findings from the first wave of a nationally representative cross-sectional survey. Prev Med (Baltim) [Internet]. 2021;145. Available from: https://www.sciencedirect.com/science/article/pii/S0091743520303649
- Footnote 150
-
Capaldi CA, Liu L, Ooi LL, Roberts KC. At-a-glance – Self-rated mental health, community belonging, life satisfaction and perceived change in mental health among adults during the second and third waves of the COVID-19 pandemic in Canada. Heal Promot Chronic Dis Prev Canada [Internet]. 2022;42(5):218–25. Available from: https://www.canada.ca/en/public-health/services/reports-publications/health-promotion-chronic-disease-prevention-canada-research-policy-practice/vol-42-no-5-2022/self-rated-mental-health-community-belonging-life-satisfaction-perceived-change-mental-health
- Footnote 151
-
Pongou R, Ahinkorah BO, Maltais S, Mabeu MC, Agarwal A, Yaya S. Psychological distress during the COVID-19 pandemic in Canada. PLoS One. 2022;17(11 November).
- Footnote 152
-
Virgolino A, Costa J, Santos O, Pereira ME, Antunes R, Ambrosio S, et al. Lost in transition: a systematic review of the association between unemployment and mental health. J Ment Heal [Internet]. 2022;31(3):432–44. Available from: https://www.tandfonline.com/doi/pdf/10.1080/09638237.2021.2022615
- Footnote 153
-
Canadian Human Rights Commission. What is discrimination? [Internet]. 2023 [cited 2023 Dec 19]. Available from: https://www.chrc-ccdp.gc.ca/en/about-human-rights/what-discrimination
- Footnote 154
-
Statistics Canada. Quality of Life Framework for Canada [Internet]. 2022 [cited 2023 Dec 18]. Available from: https://www160.statcan.gc.ca/about-apropos-eng.htm
- Footnote 155
-
Harnois CE, Bastos JL, Shariff-Marco S. Intersectionality, Contextual Specificity, and Everyday Discrimination: Assessing the Difficulty Associated With Identifying a Main Reason for Discrimination Among Racial/Ethnic Minority Respondents. Sociol Methods Res. 2022;51(3).
- Footnote 156
-
Vargas SM, Huey SJ, Miranda J. A critical review of current evidence on multiple types of discrimination and mental health. Am J Orthopsychiatry. 2020;90(3).
- Footnote 157
-
Williams MT, Khanna Roy A, MacIntyre MP, Faber S. The Traumatizing Impact of Racism in Canadians of Colour. Vol. 8, Current Trauma Reports. 2022.
- Footnote 158
-
Mooten N. Racism, Discrimination and Migrant Workers in Canada: Evidence from the Literature [Internet]. Ottawa, ON; 2021. Available from: https://www.canada.ca/content/dam/ircc/documents/pdf/english/corporate/reports-statistics/research/racism/r8-2020-racism-eng.pdf
- Footnote 159
-
Williams DR, Mohammed SA. Racism and health I: Pathways and scientific evidence. Am Behav Sci. 2013;57(8):1152–73.
- Footnote 160
-
Braveman PA, Arkin E, Proctor D, Kauh T, Holm N. Systemic And Structural Racism: Definitions, Examples, Health Damages, And Approaches To Dismantling: Study examines definitions, examples, health damages, and dismantling systemic and structural racism. Health Aff. 2022;41(2):171–8.
- Footnote 161
-
Krieger N. Discrimination and health inequities. Int J Heal Serv. 2014;44(4):643–710.
- Footnote 162
-
Paradies Y, Ben J, Denson N, Elias A, Priest N, Pieterse A, et al. Racism as a determinant of health: a systematic review and meta-analysis. PLoS One. 2015;10(9):e0138511.
- Footnote 163
-
Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Vol. 389, The Lancet. 2017.
- Footnote 164
-
Cénat JM. Complex Racial Trauma: Evidence, Theory, Assessment, and Treatment. Perspect Psychol Sci. 2023;18(3).
- Footnote 165
-
Phelan JC, Link BG. Is Racism a Fundamental Cause of Inequalities in Health? Annu Rev Sociol. 2015;41.
- Footnote 166
-
Cénat JM, Kogan C, Noorishad PG, Hajizadeh S, Dalexis RD, Ndengeyingoma A, et al. Prevalence and correlates of depression among Black individuals in Canada: The major role of everyday racial discrimination. Depress Anxiety. 2021;38(9).
- Footnote 167
-
Salami B, Idi Y, Anyieth Y, Cyuzuzo L, Denga B, Alaazi D, et al. Factors that contribute to the mental health of Black youth. C Can Med Assoc J. 2022;194(41).
- Footnote 168
-
Suleman S, Garber KD, Rutkow L. Xenophobia as a determinant of health: an integrative review. J Public Health Policy. 2018;39:407–23.
- Footnote 169
-
Ontario Human Rights Commission. Ontario Human Rights Commission: Xenophobia [Internet]. 2023 [cited 2023 Dec 18]. Available from: https://www.ohrc.on.ca/en/policy-preventing-discrimination-based-creed/3-background#:~:text=Xenophobia describes “attitudes%2C prejudices and,%2C society or national identity.”
- Footnote 170
-
Walks RA, Bourne LS. Ghettos in Canada’s cities? Racial segregation, ethnic enclaves and poverty concentration in Canadian urban areas. Can Geogr. 2006;50(3).
- Footnote 171
-
Hodge DR, Limb GE, Cross TL. Moving from colonization toward balance and harmony: A native American perspective on wellness. Soc Work. 2009;54(3).
- Footnote 172
-
Allan B, Smylie J. First Peoples, Second Class Treatment. First Peoples, Second Cl Treat Role Racism Heal Well-being Indig Peoples Canada. 2015;
- Footnote 173
-
Woolford A. DISCIPLINE, TERRITORY, AND THE COLONIAL MESH: Colon Genocide Indig North Am. 2021 May 12;29–48.
- Footnote 174
-
Dussault R, Erasmus G. Report of the royal commission on aboriginal peoples. 1996;
- Footnote 175
-
Waldram JB, Herring A, Young TK. Aboriginal health in Canada: Historical, cultural, and epidemiological perspectives. University of Toronto Press; 2006.
- Footnote 176
-
Government of Canada. First Nations in Canada [Internet]. 2017 [cited 2023 Sep 22]. Available from: https://www.rcaanc-cirnac.gc.ca/eng/1307460755710/1536862806124
- Footnote 177
-
Wheeler W. Colonialism and First Nations Women. In: Dua E, Roberts A, editors. Scratching the Surface: Canadian Anti-Racist Feminist Thought. Toronto: Women’s Press; 1999. p. 49–80.
- Footnote 178
-
Luby B, Labelle K. “The New Generation”: Cooperative Education at the Day School on Dalles 38C Indian Reserve, 1890-1910. Ont Hist [Internet]. 2015 Oct [cited 2023 Dec 19];107(1):88–110. Available from: https://id.erudit.org/iderudit/1050680ar
- Footnote 179
-
Truth and Reconciliation Commission of Canada. The survivors speak: a report of the Truth and Reconciliation Commission of Canada. Truth Reconcil Comm Canada. 2015;
- Footnote 180
-
Government of Canada. Apology for the Inuit High Arctic relocation [Internet]. 2010 [cited 2023 Dec 19]. Available from: https://www.rcaanc-cirnac.gc.ca/eng/1100100016115/1534786491628
- Footnote 181
-
Tester FJ. Mad dogs and (mostly) Englishmen: Colonial relations, commodities, and the fate of Inuit sled dogs. Études/Inuit/Studies. 2011;34(2).
- Footnote 182
-
Government of Canada. Government of Canada’s apology to Qikiqtani Inuit [Internet]. 2019 [cited 2023 Dec 19]. Available from: https://www.rcaanc-cirnac.gc.ca/eng/1565717416770/1565717444492
- Footnote 183
-
Olofsson E, Holton TL, Partridge I “Jacob.” Negotiating identities: Inuit tuberculosis evacuees in the 1940s-1950s. Études/Inuit/Studies. 2009;32(2).
- Footnote 184
-
Auger MD. “We need to not be footnotes anymore”: understanding Metis people’s experiences with mental health and wellness in British Columbia, Canada. Public Health [Internet]. 2019;176:92–7. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med16&NEWS=N&AN=30678887
- Footnote 185
-
Logan T. Settler colonialism in Canada and the Métis. J Genocide Res [Internet]. 2015 Oct 2 [cited 2024 Feb 9];17(4):433–52. Available from: https://www.tandfonline.com/doi/abs/10.1080/14623528.2015.1096589
- Footnote 186
-
The Aboriginal Healing Foundation. Métis History and Experience and Residential Schools in Canada. Education. 2006.
- Footnote 187
-
A. B, K. M, H. A. The intergenerational effects of Indian Residential Schools: Implications for the concept of historical trauma. Transcult Psychiatry. 2014;51(3).
- Footnote 188
-
Hunt B, Wilson CL, Fauzia G, Mazhar F. The Muslimah Project: A Collaborative Inquiry into Discrimination and Muslim Women’s Mental Health in a Canadian Context. Am J Community Psychol. 2020;66(3–4).
- Footnote 189
-
Wilkins‐Laflamme S. Islamophobia in Canada: Measuring the realities of negative attitudes toward Muslims and religious discrimination. Can Rev Sociol Can Sociol. 2018;55(1):86–110.
- Footnote 190
-
Senate Canada. Combatting Hate: Islamophobia and its Impact on Muslims in Canada [Internet]. 2023. Available from: https://sencanada.ca/content/sen/committee/441/RIDR/reports/Islamophobia_FINAL_e.pdf
- Footnote 191
-
Razack S. Looking White People in the Eye: Gender, Race and Culture in the Courtroom and Classrooms. Toronto, Canada: University of Toronto Press; 1998. 1–205 p.
- Footnote 192
-
Statistics Canada. Table 35-10-0066-01 Police-reported hate crime, by type of motivation, Canada (selected police services). 2023.
- Footnote 193
-
Mamdani M. Good Muslim, bad Muslim: A political perspective on culture and terrorism. Am Anthropol. 2002;104(3):766–75.
- Footnote 194
-
Woodlock R. Identity and Islamophobia: An Australian Investigation. Fear Muslims? Int Perspect Islam. 2016;131–51.
- Footnote 195
-
National Collaborating Centre for Determinants of Health. Let’s Talk: Racism and Health Equity (Rev. ed.). Antigonish, Nova Scotia; 2018.
- Footnote 196
-
Law S, Andermann L, Chow W, Luo XW, Wang X. Experiences of Family Burden in Caring for the Severely Mentally Ill in a Foreign Land: A Qualitative Study of Chinese Immigrant Families in Toronto, Canada. Transcult Psychiatry. 2021;58(6).
- Footnote 197
-
O’Mahony JM, Donnelly TT. How does gender influence immigrant and refugee women’s postpartum depression help-seeking experiences? J Psychiatr Ment Health Nurs [Internet]. 2013;20(8):714–25. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med10&NEWS=N&AN=22962942
- Footnote 198
-
Whitehead M, Dahlgren G, Whitehead M, WHO. Concepts and principles for tackling social inequities in health : Levelling up Part 1. World Heal Organ. 2007;(2).
- Footnote 199
-
Aguinaldo JP. The social construction of gay oppression as a determinant of gay men’s health:‘Homophobia is killing us.’ Crit Public Health. 2008;18(1):87–96.
- Footnote 200
-
Kitzinger C. Sexualities. In: Handbook of the psychology of women and gender. Hoboken, NJ, US: John Wiley & Sons, Inc.; 2001. p. 272–85.
- Footnote 201
-
Jaffray B. Experiences of violent victimization and unwanted sexual behaviours among gay, lesbian, bisexual and other sexual minority people, and the transgender population, in Canada, 2018. Juristat Can Cent Justice Stat. 2020;1–27.
- Footnote 202
-
Oliffe JL, Kelly MT, Montaner GG, Links PS, Kealy D, Ogrodniczuk JS. Segmenting or summing the parts? A scoping review of male suicide research in Canada. Can J Psychiatry. 2021;66(5):433–45.
- Footnote 203
-
Crenshaw K. Demarginalizing the intersection of race and sex: A black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. Univ Chic Leg Forum. 1989;139:139–67.
- Footnote 204
-
Dhamoon RK. Considerations on mainstreaming intersectionality. Polit Res Q [Internet]. 2011 Sep 22;64(1):230–43. Available from: https://doi.org/10.1177/1065912910379227
- Footnote 205
-
Hancock AM. When multiplication doesn’t equal quick addition: Examining intersectionality as a research paradigm. Perspect Polit. 2007;5(1):63–79.
- Footnote 206
-
Meyer IH. Prejudice, Social Stress, and Mental Health in Lesbian, Gay, and Bisexual Populations: Conceptual Issues and Research Evidence. Vol. 129, Psychological Bulletin. 2003. p. 674–97.
- Footnote 207
-
Kinitz DJ, Goodyear T, Dromer E, Gesink D, Ferlatte O, Knight R, et al. “Conversion Therapy” Experiences in Their Social Contexts: A Qualitative Study of Sexual Orientation and Gender Identity and Expression Change Efforts in Canada. Can J Psychiatry. 2022;67(6).
- Footnote 208
-
Statistics Canada. Survey of Safety in Public and Private Spaces (SSPPS) [Internet]. 2019 [cited 2023 Dec 18]. Available from: https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=5256
- Footnote 209
-
Lewis NM. Rupture, resilience, and risk: Relationships between mental health and migration among gay-identified men in North America. Heal Place. 2014;27.
- Footnote 210
-
Logie CH, Lys C, ice L, Dias L, Schott N, Zouboules MR, et al. “Automatic assumption of your gender, sexuality and sexual practices is also discrimination”: Exploring sexual healthcare experiences and recommendations among sexually and gender diverse persons in Arctic Canada. Health Soc Care Community [Internet]. 2019;27(5):1204–13. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=psyc16&NEWS=N&AN=2019-21510-001
- Footnote 211
-
Creighton GM, Oliffe JL, Broom A, Rossnagel E, Ferlatte O, Darroch F. “I Never Saw a Future”: Childhood Trauma and Suicidality Among Sexual Minority Women. Qual Health Res [Internet]. 2019;29(14):2035–47. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med16&NEWS=N&AN=31030661
- Footnote 212
-
Lyons T, Shannon K, Pierre L, Small W, Krusi A, Kerr T. A qualitative study of transgender individuals’ experiences in residential addiction treatment settings: Stigma and inclusivity. Subst Abuse Treat Prev Policy [Internet]. 2015;10. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=psyc12&NEWS=N&AN=2015-22853-001
- Footnote 213
-
Handlovsky I, Bungay V, Oliffe J, Johnson J. Developing Resilience: Gay Men’s Response to Systemic Discrimination. Am J Mens Health. 2018;12(5).
- Footnote 214
-
Lewis NM. Moving “out,” moving on: Gay men’s migrations through the life course. Ann Assoc Am Geogr. 2014;104(2):225–33.
- Footnote 215
-
Parmenter J, Galliher R V., Maughan ADA. LGBTQ+ emerging adults perceptions of discrimination and exclusion within the LGBTQ+ community. Psychol Sex. 2021;12(4):289–304.
- Footnote 216
-
Weiss J. GL vs. BT: The Archaeology of Biphobia and Transphobia Within the U.S. Gay and Lesbian Community. In: Bisexuality and Transgenderism. 2004. p. 31.
- Footnote 217
-
Colliver B. Re-imagining Hate Crime. 2021. 223 p.
- Footnote 218
-
Mulick P, Wright Jr. L. Examining the Existence of Biphobia in the Heterosexual and Homosexual Populations. J Bisex. 2002;2(4):45–64.
- Footnote 219
-
Ross LE, Salway T, Tarasoff LA, MacKay JM, Hawkins BW, Fehr CP. Prevalence of Depression and Anxiety Among Bisexual People Compared to Gay, Lesbian, and Heterosexual Individuals:A Systematic Review and Meta-Analysis. Vol. 55, Journal of Sex Research. 2018.
- Footnote 220
-
Tebbe EA, Budge SL. Factors that drive mental health disparities and promote well-being in transgender and nonbinary people. Vol. 1, Nature Reviews Psychology. 2022.
- Footnote 221
-
Holt MK, Parodi KB, Elgar FJ, Vigna A, Moore LB, Koenig B. Identifying protective factors for gender diverse adolescents’ mental health. npj Ment Heal Res. 2023;2(1).
- Footnote 222
-
Mizock L, Woodrum D, Riley J, Sotilleo E, Yuen N, Ormerod A. Coping with transphobia in employment: Strategies used by transgender and gender-diverse people in the United States. Int J Transgenderism. 2017;18(3):282–94.
- Footnote 223
-
Ooi LL, Liu L, Roberts KC, Gariépy G, Capaldi CA. Social isolation, loneliness and positive mental health among older adults in Canada during the COVID-19 pandemic. Heal Promot Chronic Dis Prev Canada. 2023;43(4).
- Footnote 224
-
World Health Organization. Social Isolation and Loneliness [Internet]. 2023 [cited 2024 Jan 17]. Available from: https://www.who.int/teams/social-determinants-of-health/demographic-change-and-healthy-ageing/social-isolation-and-loneliness
- Footnote 225
-
Statistics Canada. The Daily. 2022 [cited 2024 Jan 17]. Home alone: More persons living solo than ever before, but roomies the fastest growing household type. Available from: https://www150.statcan.gc.ca/n1/daily-quotidien/220713/dq220713a-eng.htm
- Footnote 226
-
US Public Health Service. Our Epidemic of Loneliness and Isolation: The U.S. Surgeon General’s Advisory on the Healing Effects of Social Connection and Community [Internet]. 2023. Available from: https://www.hhs.gov/sites/default/files/surgeon-general-social-connection-advisory.pdf
- Footnote 227
-
Michalski CA, Diemert LM, Helliwell JF, Goel V, Rosella LC. Relationship between sense of community belonging and self-rated health across life stages. SSM - Popul Heal. 2020;12.
- Footnote 228
-
Logie CH, Lacombe-Duncan A, Lee-Foon N, Ryan S, Ramsay H. “It’s for us -newcomers, LGBTQ persons, and HIV-positive persons. You feel free to be”: A qualitative study exploring social support group participation among African and Caribbean lesbian, gay, bisexual and transgender newcomers and refugees in Toronto, Canada. BMC Int Health Hum Rights. 2016;16(1).
- Footnote 229
-
Canadian Mental Health Association. Feeling well includes feeling like you belong [Internet]. 2021. Available from: https://cmha.ca/news/feeling-well-includes-feeling-like-you-belong/
- Footnote 230
-
Sherman ADF, Clark KD, Robinson K, Noorani T, Poteat T. Trans ∗ Community Connection, Health, and Wellbeing: A Systematic Review. Vol. 7, LGBT Health. 2020.
- Footnote 231
-
Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Soc Sci Med [Internet]. 2000;51(6):843–57. Available from: https://pubmed.ncbi.nlm.nih.gov/10972429/
- Footnote 232
-
Statistics Canada. Almost half of Canadians report a strong sense of belonging to their local community [Internet]. Ottawa, ON; 2022. Available from: https://www150.statcan.gc.ca/n1/en/daily-quotidien/220819/dq220819b-eng.pdf?st=ULuS80e4
- Footnote 233
-
Salami B, Salma J, Hegadoren K, Meherali S, Kolawole T, Diaz E. Sense of community belonging among immigrants: Perspective of immigrant service providers. Public Health [Internet]. 2019;167:28–33. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=psyc16&NEWS=N&AN=2019-08551-006
- Footnote 234
-
Kitchen P, Williams AM, Gallina M. Sense of belonging to local community in small-to-medium sized Canadian urban areas: a comparison of immigrant and Canadian-born residents. BMC Psychol [Internet]. 2015;3. Available from: https://link.springer.com/article/10.1186/s40359-015-0085-0
- Footnote 235
-
Pitt RS, Sherman J, Macdonald ME. Low-income working immigrant families in Quebec: Exploring their challenges to well-being. Can J Public Heal [Internet]. 2015;106:539–45. Available from: https://link.springer.com/article/10.17269/CJPH.106.5028
- Footnote 236
-
Kim IH, Carrasco C, Muntaner C, McKenzie K, Noh S. Ethnicity and Postmigration Health Trajectory in New Immigrants to Canada. Am J Public Health [Internet]. 2013;103(4):96–104. Available from: https://ajph.aphapublications.org/doi/full/10.2105/AJPH.2012.301185
- Footnote 237
-
Chadwick KA, Collins PA. Examining the relationship between social support availability, urban center size, and self-perceived mental health of recent immigrants to Canada: A mixed-methods analysis. Soc Sci Med [Internet]. 2015;128:220–30. Available from: https://www.sciencedirect.com/science/article/pii/S0277953615000623
- Footnote 238
-
Public Health Agency of Canada (PHAC). Mobilizing Public Health Action on Climate Change in Canada: CPHO 2022 Report. 2022.
- Footnote 239
-
Statistics Canada. Immigrants’ sense of belonging to Canada by province of residence [Internet]. 2023. Available from: https://www150.statcan.gc.ca/n1/en/pub/36-28-0001/2023006/article/00003-eng.pdf?st=rjJzBmdz
- Footnote 240
-
Pilling M, Howison M, Frederick T, Ross L, Bellamy CD, Davidson L, et al. Fragmented inclusion: Community participation and lesbian, gay, bisexual, trans, and queer people with diagnoses of schizophrenia and bipolar disorder. Am J Orthopsychiatry [Internet]. 2017;87(5):606–13. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med14&NEWS=N&AN=28253016
- Footnote 241
-
Ford JD, Berrang-Ford L, King M, Furgal C. Vulnerability of Aboriginal health systems in Canada to climate change. Glob Environ Chang [Internet]. 2010;20(4):668–80. Available from: http://dx.doi.org/10.1016/j.gloenvcha.2010.05.003
- Footnote 242
-
Dodd W, Scott P, Howard C, Scott C, Rose C, Cunsolo A, et al. Lived experience of a record wildfire season in the Northwest Territories, Canada. Can J Public Heal. 2018 Jun 1;109(3):327–37.
- Footnote 243
-
Government of Canada. Climate change concepts [Internet]. Ottawa, ON; 2020. Available from: https://www.canada.ca/en/environment-climate-change/services/climate-change/canadian-centre-climate-services/basics/concepts.html#shr-pg0
- Footnote 244
-
Cunsolo AW, Harper SL, Ford JD, Edge VL, Landman K, Houle K, et al. Climate change and mental health: An exploratory case study from Rigolet, Nunatsiavut, Canada. Clim Change. 2013 Nov;121(2):255–70.
- Footnote 245
-
Health Canada. Health of Canadians in a Changing Climate: Advancing our Knowledge for Action. 2022.
- Footnote 246
-
Cunsolo A, Borish D, Harper SL, Snook J, Shiwak I, Wood M. “You can never replace the caribou”: Inuit Experiences of Ecological Grief from Caribou Declines. Am Imago. 2020 Mar 1;77(1):31–59.
- Footnote 247
-
Sawatzky A, Cunsolo A, Jones-Bitton A, Gillis D, Wood M, Flowers C, et al. “The best scientists are the people that’s out there”: Inuit-led integrated environment and health monitoring to respond to climate change in the Circumpolar North. Clim Change. 2020 May 1;160(1):45–66.
- Footnote 248
-
Middleton J, Cunsolo A, Jones-Bitton A, Shiwak I, Wood M, Pollock N, et al. “We’re people of the snow:” Weather, climate change, and Inuit mental wellness. Soc Sci Med. 2020 Oct 1;262.
- Footnote 249
-
Petrasek MacDonald J, Harper SL, Cunsolo Willox A, Edge VL. A necessary voice: Climate change and lived experiences of youth in Rigolet, Nunatsiavut, Canada. Glob Environ Chang. 2013 Feb;23(1):360–71.
- Footnote 250
-
Boulanger-Lapointe N, Gérin-Lajoie J, Siegwart Collier L, Desrosiers S, Spiech C, Henry GHR, et al. Berry Plants and Berry Picking in Inuit Nunangat: Traditions in a Changing Socio-Ecological Landscape. Hum Ecol. 2019 Feb 1;47(1):81–93.
- Footnote 251
-
Gilbert SZ, Walsh DE, Levy SN, Maksagak B, Milton MI, Ford JD, et al. Determinants, effects, and coping strategies for low-yield periods of harvest: a qualitative study in two communities in Nunavut, Canada. Food Secur [Internet]. 2021;13:157–79. Available from: https://doi.org/10.1007/s12571-020-01112-0
- Footnote 252
-
Newell SL, Doubleday NC. Sharing country food: connecting health, food security and cultural continuity in Chesterfield Inlet, Nunavut. Polar Res. 2020 Dec 18;39.
- Footnote 253
-
Panikkar B, Lemmond B. Being on land and sea in troubled times: Climate change and food sovereignty in Nunavut. Land. 2020 Dec 1;9(12):1–18.
- Footnote 254
-
Sansoulet J, Therrien M, Delgove J, Pouxviel G, Desriac J, Sardet N, et al. An update on Inuit perceptions of their changing environment, Qikiqtaaluk (Baffin Island, Nunavut). Elementa. 2020 Nov 2;8(1).
- Footnote 255
-
Petrasek MacDonald J, Cunsolo Willox A, Ford JD, Shiwak I, Wood M, Wolfrey C, et al. Protective factors for mental health and well-being in a changing climate: Perspectives from Inuit youth in Nunatsiavut, Labrador. Soc Sci Med. 2015 Sep 1;141:133–41.
- Footnote 256
-
Cunsolo AW, Harper SL, Ford JD, Landman K, Houle K, Edge VL. “From this place and of this place:” Climate change, sense of place, and health in Nunatsiavut, Canada. Soc Sci Med. 2012 Aug;75(3):538–47.
- Footnote 257
-
Cunsolo AW, Harper SL, Edge VL, Landman K, Houle K, Ford JD. The land enriches the soul: On climatic and environmental change, affect, and emotional health and well-being in Rigolet, Nunatsiavut, Canada. Emot Sp Soc. 2013 Feb;6(1):14–24.
- Footnote 258
-
Proverbs TA, Lantz TC, Lord SI, Amos A, Ban NC. Social-Ecological Determinants of Access to Fish and Well-Being in Four Gwich’in Communities in Canada’s Northwest Territories. Hum Ecol. 2020 Apr 1;48(2):155–71.
- Footnote 259
-
Ironside A, Ferguson LJ, Katapally TR, Foulds HJA. Cultural connectedness as a determinant of physical activity among Indigenous adults in Saskatchewan. Appl Physiol Nutr Metab [Internet]. 2020 [cited 2023 Sep 7];45(9):937–47. Available from: https://cdnsciencepub.com/doi/10.1139/apnm-2019-0793
- Footnote 260
-
Snowshoe A, Crooks C V., Tremblay PF, Hinson RE. Cultural Connectedness and Its Relation to Mental Wellness for First Nations Youth. J Prim Prev. 2017;38(1–2).
- Footnote 261
-
Herkimer J, Earle M. The Importance of Indigenous Languages: An Investigation of Sense of Belonging and Mental Health Among Students and Non-Students [Internet]. 2022. Available from: https://indspire.ca/wp-content/uploads/2023/03/The-Importance-of-Indigenous-Languages-An-Investigation-of-Sense-of-Belonging-and-Mental-Health-Among-Students-and-Non-Students-FINAL.pdf
- Footnote 262
-
Burnett C, Purkey E, Davison CM, Watson A, Kehoe J, Traviss S, et al. Spirituality, Community Belonging, and Mental Health Outcomes of Indigenous Peoples during the COVID-19 Pandemic. Int J Environ Res Public Health. 2022;19(4).
- Footnote 263
-
Wilkinson RG, Marmot M. Social Determinants of Health: The Solid Facts Second Edition [Internet]. 2003. Available from: https://apps.who.int/iris/bitstream/handle/10665/326568/9789289013710-eng.pdf?sequence=1&isAllowed=y
- Footnote 264
-
Kirmayer LJ, Brass GM, Tait CL. The Mental Health of Aboriginal Peoples: Transformations of Identity and Community. http://dx.doi.org/101177/070674370004500702 [Internet]. 2000 Sep 1 [cited 2023 Sep 7];45(7):607–16. Available from: https://journals.sagepub.com/doi/abs/10.1177/070674370004500702
- Footnote 265
-
Charles G, DeGagné M. Student-to-Student Abuse in the Indian Residential Schools in Canada: Setting the Stage for Further Understanding. http://dx.doi.org/101080/0145935X2013859903 [Internet]. 2013 [cited 2023 Sep 7];34(4):343–59. Available from: https://www.tandfonline.com/doi/abs/10.1080/0145935X.2013.859903
- Footnote 266
-
Greenwood M, de Leeuw S, Linday NM, Reading C. Determinants of Indigenous Peoples’ Health in Canada: Beyond the Social. Toronto, ON: Canadian Scholars; 2015.
- Footnote 267
-
Cao L, Burton VS, Liu L. Correlates of Illicit Drug Use Among Indigenous Peoples in Canada: A Test of Social Support Theory. Int J Offender Ther Comp Criminol [Internet]. 2018 Oct 1 [cited 2023 Sep 7];62(14):4510–27. Available from: https://pubmed.ncbi.nlm.nih.gov/29484913/
- Footnote 268
-
Reading CL, Wein F. Health Inequalities and Social Determinants of Aboriginal Peoples’ Health. Natl Collab Cent Aborig Heal. 2009;
- Footnote 269
-
Spillane NS, Schick MR, Kirk-Provencher KT, Nalven T, Goldstein SC, Crawford MC, et al. Trauma and Substance Use among Indigenous Peoples of the United States and Canada: A Scoping Review. https://doi.org/101177/15248380221126184 [Internet]. 2022 Oct 5 [cited 2023 Sep 8]; Available from: https://journals.sagepub.com/doi/10.1177/15248380221126184
- Footnote 270
-
Tousignant M, Sioui N. Resilience and Aboriginal Communities in Crisis: Theory and Interventions. J Aborig Heal. 2009;5(1).
- Footnote 271
-
Parker L, Jamous M, Marek R, Camacho C. Traditions and innovations: a community-based approach to substance abuse prevention. Vol. 74, Rhode Island medical journal. 1991.
- Footnote 272
-
Martin D, Miller AP, Quesnel-Vallée A, Caron NR, Vissandjée B, Marchildon GP. Canada’s universal health-care system: achieving its potential. Vol. 391, The Lancet. 2018.
- Footnote 273
-
Bartram M, Leslie K, Atanackovic J, Tulk C, Chamberland-Rowe C, Bourgeault IL. Out from the shadows: What health leaders should do to advance the mental health and substance use health workforce. Healthc Manag Forum. 2023;36(1).
- Footnote 274
-
CMHA. Budget 2023 out of touch with mental health crisis. 2023.
- Footnote 275
-
Lang K, El-Aneed A, Berenbaum S, Dell CA, Wright J, McKay ZT. Qualitative assessment of crisis services among persons using injection drugs in the city of Saskatoon. J Subst Use [Internet]. 2013;18(1):3–11. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=psyc10&NEWS=N&AN=2013-03222-002
- Footnote 276
-
Luongo NM. Disappearing in plain sight: An exploratory study of co-occurring eating and substance abuse dis/orders among homeless youth in Vancouver, Canada. Womens Stud Int Forum [Internet]. 2018;67:38–44. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=psyc15&NEWS=N&AN=2018-12354-007
- Footnote 277
-
McCutcheon JM, Morrison MA. Injecting on the Island: A qualitative exploration of the service needs of persons who inject drugs in Prince Edward Island, Canada. Harm Reduct J. 2014;11(1).
- Footnote 278
-
Ross LE, Vigod S, Wishart J, Waese M, Spence JD, Oliver J, et al. Barriers and facilitators to primary care for people with mental health and/or substance use issues: a qualitative study. BMC Fam Pract [Internet]. 2015;16:135. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med12&NEWS=N&AN=26463083
- Footnote 279
-
Voon P, Greer AM, Amlani A, Newman C, Burmeister C, Buxton JA. Pain as a risk factor for substance use: A qualitative study of people who use drugs in British Columbia, Canada. Harm Reduct J. 2018;15(1).
- Footnote 280
-
National Collaborating Centre for Indigenous Health. Access to Health Services as a Social Determinant of First Nations, Inuit, and Métis health [Internet]. 2019. Available from: https://www.nccih.ca/docs/determinants/FS-AccessHealthServicesSDOH-2019-EN.pdf
- Footnote 281
-
Oliffe JL, Broom A, Popa M, Jenkins EK, Rice SM, Ferlatte O, et al. Unpacking Social Isolation in Men’s Suicidality. Qual Health Res. 2019;29(3).
- Footnote 282
-
Boyd J, Fast D, Hobbins M, McNeil R, Small W. Social-structural factors influencing periods of injection cessation among marginalized youth who inject drugs in Vancouver, Canada: An ethno-epidemiological study. Harm Reduct J. 2017;14(1).
- Footnote 283
-
Caragata L, Liegghio M. Mental Health, Welfare Reliance, and Lone Motherhood. Can J Community Ment Heal [Internet]. 2013;32(1):95–107. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=psyc10&NEWS=N&AN=2014-03019-007
- Footnote 284
-
Bungay V. Health care among street-involved women: The perpetuation of health inequity. Qual Health Res. 2013;23(8).
- Footnote 285
-
Islam F, Multani A, Hynie M, Shakya Y, McKenzie K. Mental health of South Asian youth in Peel Region, Toronto, Canada: a qualitative study of determinants, coping strategies and service access. BMJ Open [Internet]. 2017;7(11):e018265. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med14&NEWS=N&AN=29101148
- Footnote 286
-
Gaspar M, Marshall Z, Rodrigues R, Adam BD, Brennan DJ, Hart TA, et al. Mental health and structural harm: a qualitative study of sexual minority men’s experiences of mental healthcare in Toronto, Canada. Cult Heal Sex [Internet]. 2021;23(1):98–114. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med19&NEWS=N&AN=31794349
- Footnote 287
-
Kerman N, Manoni-Millar S, Cormier L, Cahill T, Sylvestre J. “It’s not just injecting drugs”: Supervised consumption sites and the social determinants of health. Drug Alcohol Depend [Internet]. 2020;213. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=psyc17&NEWS=N&AN=2020-54702-001
- Footnote 288
-
Torchalla I, Linden IA, Strehlau V, Neilson EK, Krausz M. “Like a lots happened with my whole childhood”: Violence, trauma, and addiction in pregnant and postpartum women from Vancouver’s Downtown Eastside: Erratum. Harm Reduct J [Internet]. 2017;14. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=psyc14&NEWS=N&AN=2017-42462-001"
- Footnote 289
-
Taylor P. System Entrapment: Dehumanization While Help-Seeking for Suicidality in Women Who Have Experienced Intimate Partner Violence. Qual Health Res [Internet]. 2020;30(4):530–46. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med18&NEWS=N&AN=31303117
- Footnote 290
-
Furlotte C, Schwartz K. Mental Health Experiences of Older Adults Living with HIV: Uncertainty, Stigma, and Approaches to Resilience. Can J Aging [Internet]. 2017;36(2):125–40. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med14&NEWS=N&AN=28349859
- Footnote 291
-
Government of Canada. Chief Public Health Officer Health Professional Forum. 2023 [cited 2024 Feb 7]. Common Definitions on Cultural Safety: Chief Public Health Officer Health Professional Forum. Available from: https://www.canada.ca/en/health-canada/services/publications/health-system-services/chief-public-health-officer-health-professional-forum-common-definitions-cultural-safety.html
- Footnote 292
-
Baba L. Cultural safety in First Nations, Inuit and Métis public health: Environmental scan of cultural competency and safety in education, training and health services [Internet]. Prince George, BC; 2013. Available from: https://www.ccnsa-nccah.ca/docs/emerging/RPT-CulturalSafetyPublicHealth-Baba-EN.pdf
- Footnote 293
-
Reynolds K, Medved M, Mackenzie CS, Funk LM, Koven L. Older Adults’ Narratives of Seeking Mental Health Treatment: Making Sense of Mental Health Challenges and “Muddling Through” to Care. Qual Health Res [Internet]. 2020;30(10):1517–28. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med19&NEWS=N&AN=32452302
- Footnote 294
-
Gilmer C, Buccieri K. Homeless Patients Associate Clinician Bias With Suboptimal Care for Mental Illness, Addictions, and Chronic Pain. J Prim Care Community Health [Internet]. 2020;11:2150132720910289. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med18&NEWS=N&AN=32133906
- Footnote 295
-
Boyd J, Collins A, ra B, Mayer S, Maher L, Kerr T, et al. Gendered violence and overdose prevention sites: a rapid ethnographic study during an overdose epidemic in Vancouver, Canada. Addiction [Internet]. 2018;113(12):2261–70. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med15&NEWS=N&AN=30211453
- Footnote 296
-
Salami B, Denga B, Taylor R, Ajayi N, Jackson M, Asefaw M, et al. Access to mental health for Black youths in Alberta. Heal Promot chronic Dis Prev Canada Res policy Pract [Internet]. 2021;41(9):245–53. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med19&NEWS=N&AN=34549916
- Footnote 297
-
Boyd J, Lavalley J, Czechaczek S, ra, Mayer S, Kerr T, et al. “Bed Bugs and Beyond”: An ethnographic analysis of North America’s first women-only supervised drug consumption site. Int J Drug Policy [Internet]. 2020;78:102733. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med19&NEWS=N&AN=32247720
- Footnote 298
-
Collins A, ra B, Boyd J, Hayashi K, Cooper HLF, Goldenberg S, et al. Women’s utilization of housing-based overdose prevention sites in Vancouver, Canada: An ethnographic study. Int J Drug Policy [Internet]. 2020;76:102641. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med19&NEWS=N&AN=31887644
- Footnote 299
-
Ivsins A, Yake K. Looking beyond harm: Meaning and purpose of substance use in the lives of marginalized people who use drugs. Drugs Educ Prev Policy [Internet]. 2020;27(1):27–36. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=psyc17&NEWS=N&AN=2020-02582-003
- Footnote 300
-
CPHO. A Primer to Reduce Substance Use Stigma in the Canadian Health System. 2020.
- Footnote 301
-
Lipshutz JA, Hall JE, Penman-Aguilar A, Skillen E, Naoom S, Irune I. Leveraging Social and Structural Determinants of Health at the Centers for Disease Control and Prevention: A Systems-Level Opportunity to Improve Public Health. J Public Heal Manag Pract. 2022;28(2).
- Footnote 302
-
National Collaborating Centre for Determinants of Health. Let’s Talk: Public Health Roles for Improving Health Equity. National Collaborating Centre for Determinants of Health, St. Francis Xavier …; 2013.
- Footnote 303
-
Henrich J, Heine SJ, Norenzayan A. The weirdest people in the world? Behav Brain Sci. 2010;33(2–3):61–83.
- Footnote 304
-
Kirmayer LJ. Peace, conflict, and reconciliation: Contributions of cultural psychiatry. Vol. 47, Transcultural Psychiatry. Sage Publications Sage UK: London, England; 2010. p. 5–19.
- Footnote 305
-
Morgan C, McKenzie K, Fearon P. Society and psychosis. Society and Psychosis. 2008.
- Footnote 306
-
Rechel B. How to enhance the integration of primary care and public health? Approaches, facilitating factors and policy options. Eur Obs Heal Syst Policies, Policy Br 10. 2020;
- Footnote 307
-
Lasker RD, Committee on Medicine and Public Health NYA of M, Abramson DM. Medicine & Public Health: the Power of Collaboration. Center for the Advancement of Collaborative Strategies in Health, the New York Academy of Medicine.; 1997.
- Footnote 308
-
Government of Canada. Working together to improve health care for Canadians. 2023.
- Footnote 309
-
Webster P, Lipp A. The evolution of the WHO city health profiles: a content review. Health Promot Int. 2009;24 Suppl 1.
- Footnote 310
-
Nash DM, Brown JB, Thorpe C, Rayner J, Zwarenstein M. The Alliance for Healthier Communities as a Learning Health System for primary care: A qualitative analysis in Ontario, Canada. J Eval Clin Pract. 2022 Dec 1;28(6):1106–12.
- Footnote 311
-
Kynoch K, Ameen M, Ramis MA, Khalil H. Use of Patient-Reported Data within the Acute Healthcare Context: A Scoping Review. Vol. 19, International Journal of Environmental Research and Public Health. MDPI; 2022.
- Footnote 312
-
Pearson, Dennis. Elevating Patient Voices to Improve HIV Care: Patient-Reported Outcome Measures (PROMS) and Patient-Reported Experience Measures (PREMS) An Introduction to Patient-Reported Outcome Measures (PROMS) and Patient-Reported Experience Measures (PREMS) and their Importance, Implementation, and Application in HIV Care. Literature Overview on PROMS and PREMS. 2022.
- Footnote 313
-
McAllister A, Fritzell S, Almroth M, Harber-Aschan L, Larsson S, Burström B. How do macro-level structural determinants affect inequalities in mental health? - A systematic review of the literature. Vol. 17, International Journal for Equity in Health. BioMed Central Ltd.; 2018.
- Footnote 314
-
World Health Organization, Finland Ministry of Social Affairs. Helsinki Statement Framework for Country Action: Health in All Policies [Internet]. Geneva; 2014. Available from: https://iris.who.int/handle/10665/112636
- Footnote 315
-
Tam T. Chief Public Health Officer of Canada’s report on the state of public health in Canada 2020. From risk to resilience: an equity approach to COVID-19. Public Health Agency of Canada Ottawa; 2020.
- Footnote 316
-
Canadian Institute of Child Health. https://cichprofile.ca/. 2023. The Health of Canada’s Children and Youth.
- Footnote 317
-
Tonelli M, Tang KC, Forest PG. Canada needs a “Health in All Policies” action plan now. CMAJ. 2020 Jan 20;192(3):E61–7.
- Footnote 318
-
Kania J, Kramer M. Collective Impact. Soc Innov Rev [Internet]. 2011; Available from: https://ssir.org/articles/entry/collective_impact
- Footnote 319
-
Government of Canada. Measuring What Matters: Toward a Quality of Life Strategy for Canada. 2021.
- Footnote 320
-
Leppo K, Ollila E, Pena S, Wismar M, Cook S. Health in All Policies: Seizing opportunities, implementing policies. Health in All Policies. 2013.
- Footnote 321
-
Ministry of Social Affairs and Health. National Mental Health Strategy and Programme for Suicide Prevention 2020-2030. 2020.
- Footnote 322
-
Government of New Zealand. The Wellbeing Budget 2019 [Internet]. 2019. Available from: https://www.treasury.govt.nz/publications/wellbeing-budget/wellbeing-budget-2019#the-wellbeing-budget
- Footnote 323
-
Rose G. The Determinants of Individual Cases Sick individuals and sick populations. Vol. 30, International Journal of Epidemiology. 2001.
- Footnote 324
-
Marmot M, Allen J, Bell R, Bloomer E, Goldblatt P. WHO European review of social determinants of health and the health divide. Vol. 380, The Lancet. 2012.
- Footnote 325
-
First Nations Information Governance Centre. The First Nations Principles of OCAP® [Internet]. 2014 [cited 2023 Dec 18]. Available from: https://fnigc.ca/ocap-training/
- Footnote 326
-
Bailey P, Bernard C, Bayoumi A, Boozary A, Damba C, Dube S, et al. A Data Governance Framework for Health Care Data from Black Communities The Black Health Equity Working Group. 2021.
- Footnote 327
-
Canadian Mental Health Association. Advancing Mental Health Promotion in Canada. 2019;(May).
- Footnote 328
-
Government of Canada. Household food insecurity in Canada: Overview [Internet]. 2020 [cited 2024 Jan 12]. Available from: https://www.canada.ca/en/health-canada/services/food-nutrition/food-nutrition-surveillance/health-nutrition-surveys/canadian-community-health-survey-cchs/household-food-insecurity-canada-overview.html
- Footnote 329
-
Hayes K, Cunsolo A, Augustinavicius J, Stranberg R, Clayton S, Malik M, et al. Mental Health and Well-Being [Internet]. Ottawa, ON; 2022. Available from: https://ftp.maps.canada.ca/pub/nrcan_rncan/publications/STPublications_PublicationsST/329/329530/gid_329530.pdf